Appropriate Use of Personal Protective Equipment (PPE)
Subject: Fundamentals of Nursing

Overview
Appropriate Use of Personal Protective Equipment (PPE)
PPE are specialized clothing or equipment worn by employee for protection against infectious material. These techniques act as physical barriers and all should be worn to reduce the possibility of contamination of mucous membranes of the mouth, nose, and eyes.
Purpose of Using PPE
- To prevent spread of infectious agent from one to another (HAI).
- To protect individual from infectious material.
- To protect individual from injury.
Safely Use PPE
- Keep gloved hands away from face.
- Avoid touching or adjusting other PPE.
- Remove gloves if they become torn; perform hand hygiene before donning new gloves.
- Limit surfaces and items touched.
- Should be wear won for each patient.
Donning and Proper Removing of PPE
Sequence of use of PPE: Boot, Cap, Goggle, Mask, Gown, gloves
Sequence for Removing PPE: Gloves, Face shield or goggles, Gown, Mask or respirator
Gown
Gowns or aprons should be water impermeable to provide barrier protection. It is worn to prevent soiling of clothing when performing patient care procedures that are likely to generate splashes of blood, body fluids, secretions or excretions.
Method of Gowening
- Select appropriate size and suitable for the task.
- Hold the gown in front of you.
- Slide arms into sleeves, keeping hands at shoulder level away from the body.
- Opening should be at the back.
- Secure at neck and waist with a Velcro or ties.
- If gown is too small, use two gowns
- Gown 1 ties in front.
- Gown 2 ties in back.
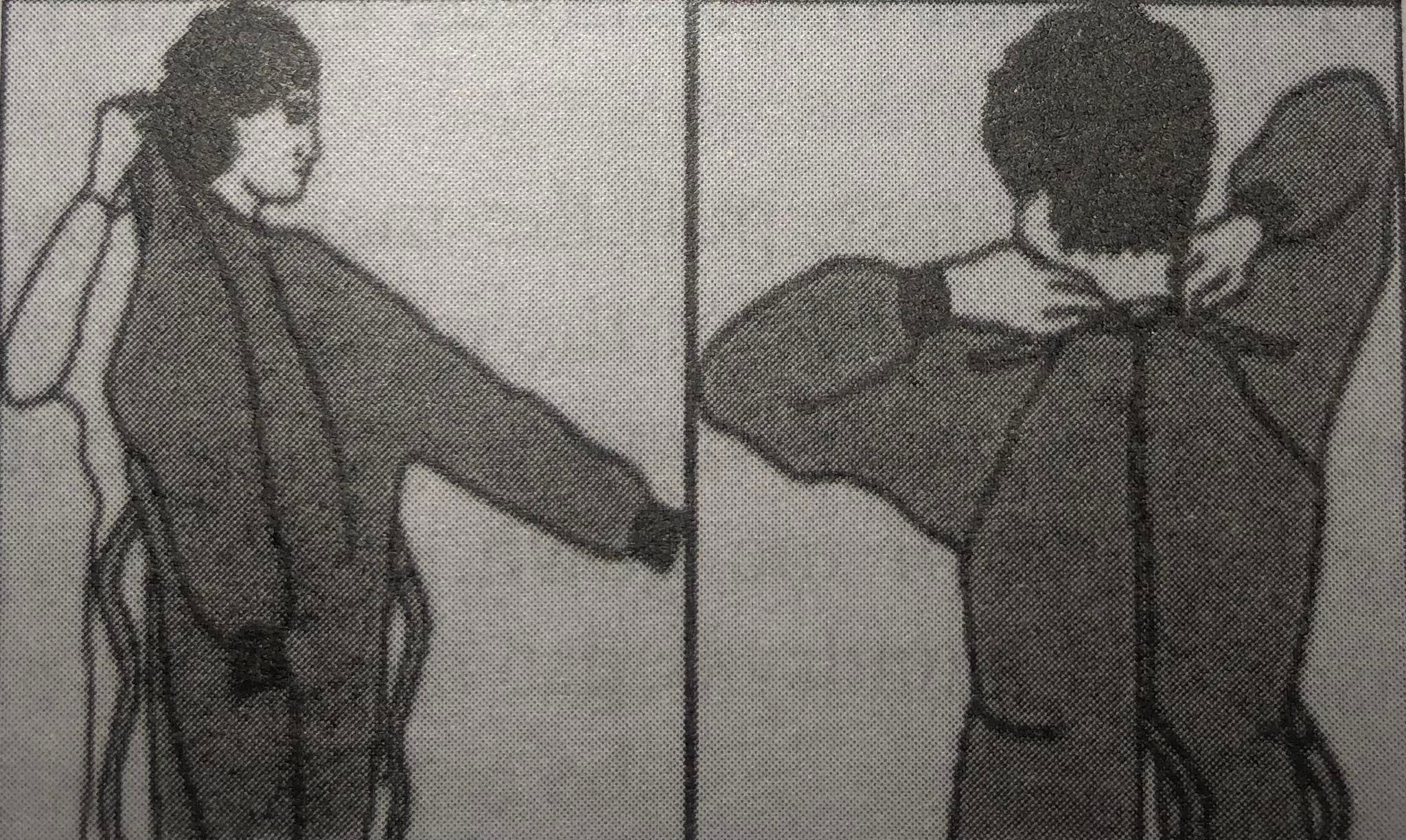
Removing a gown
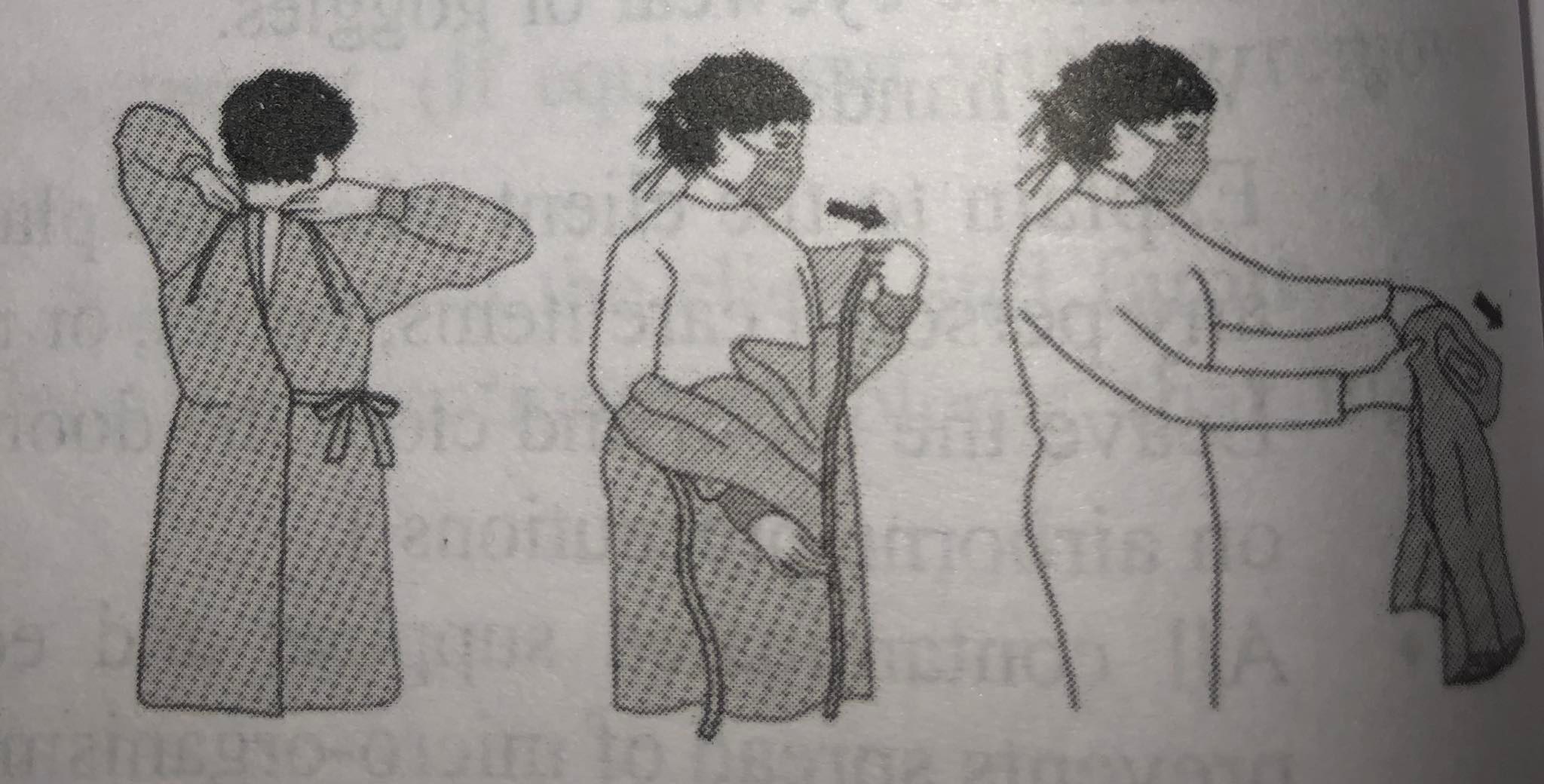
- Unfasten ties.
- Peel gown away from neck and shoulder.
- Turn contaminated outside toward the inside.
- Fold or roll into a bundle.
- Discard it into designated receptacle.
Masks
Masks provide barrier protection against splashes and sprays, and airborne droplets. Masks come in various types depending on their permeability to airborne particles. It was first used by the French surgeon Paul Berger during an operation in 1879 in Paris.
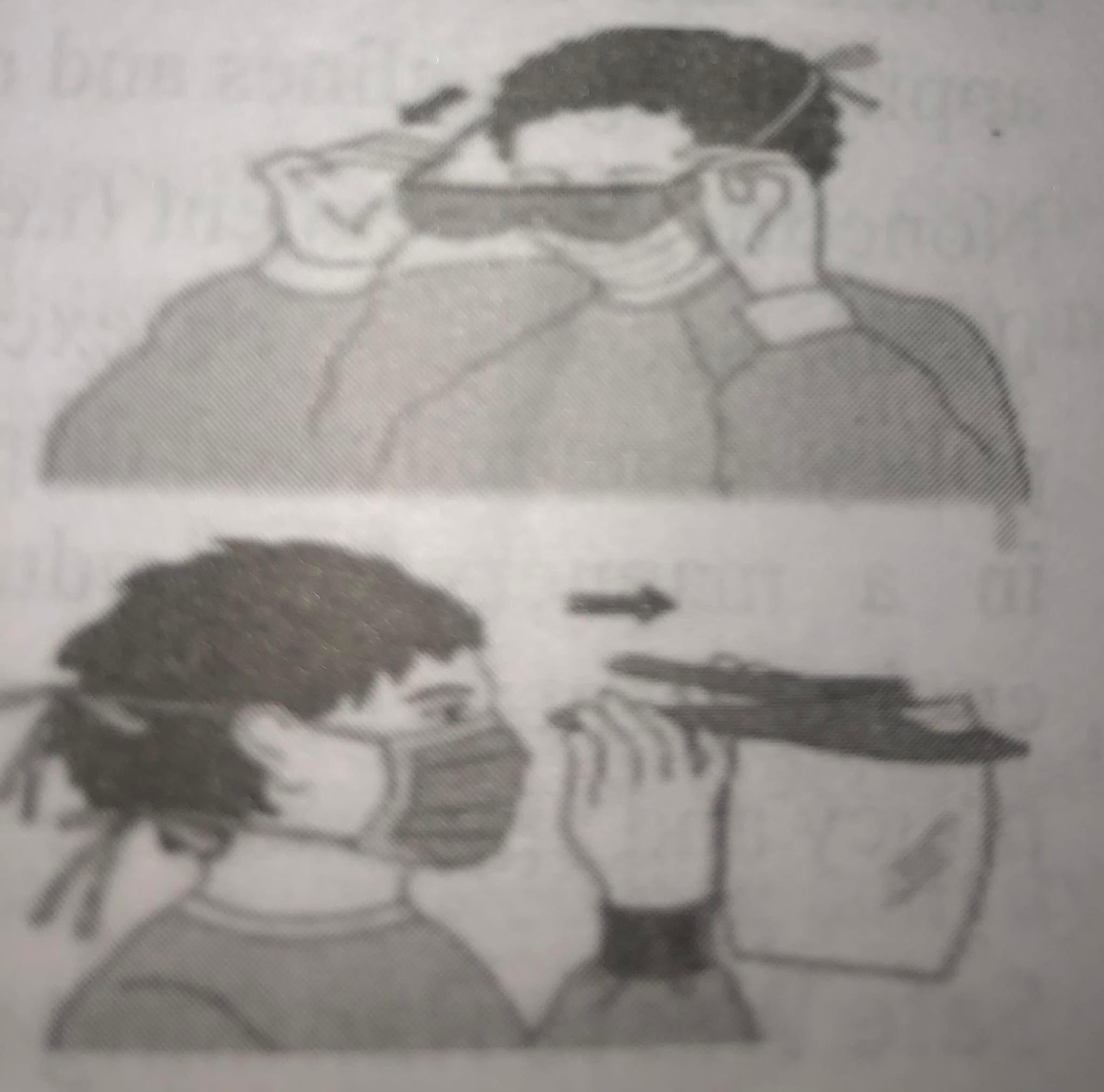
Method of Using Mask
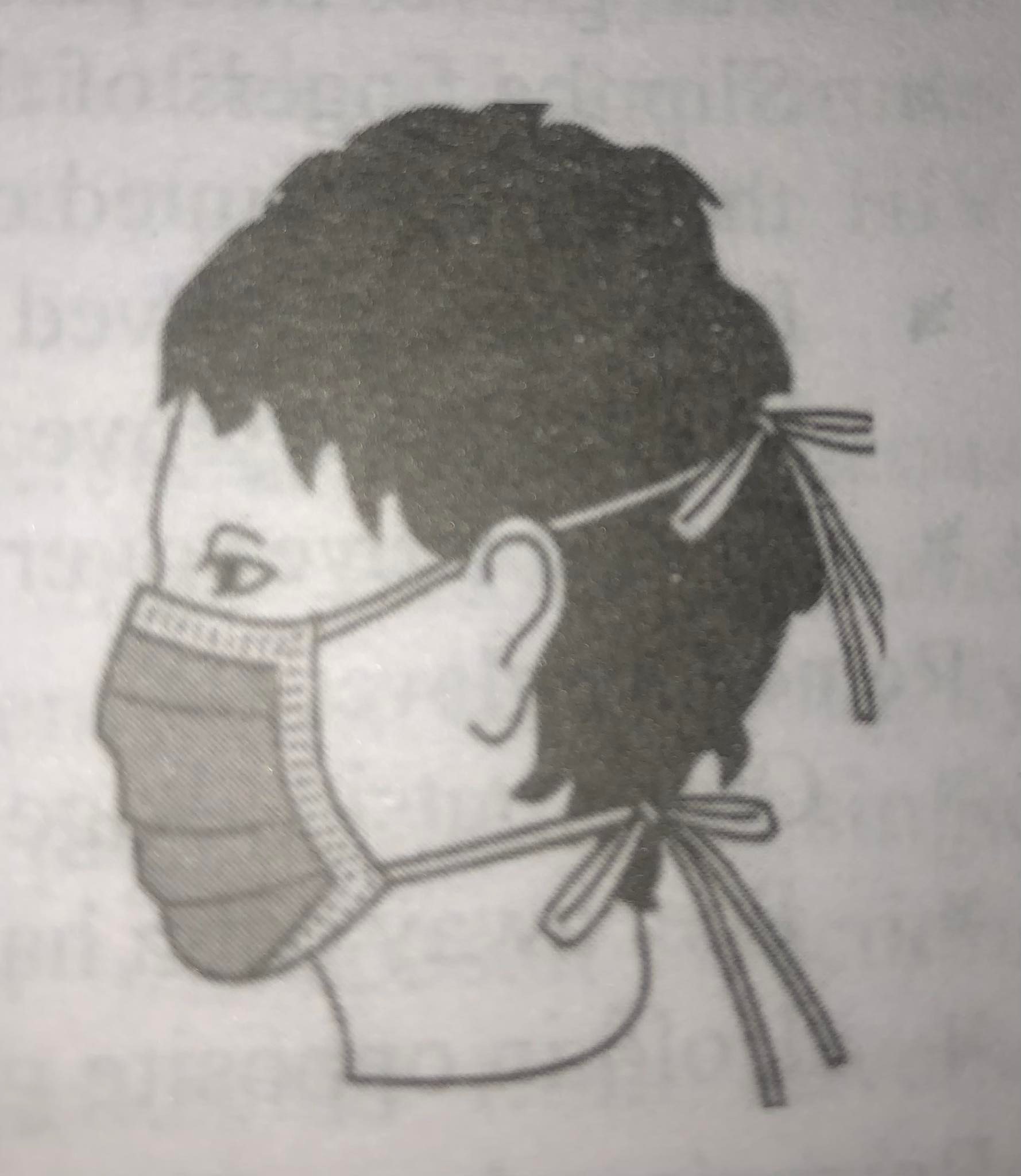
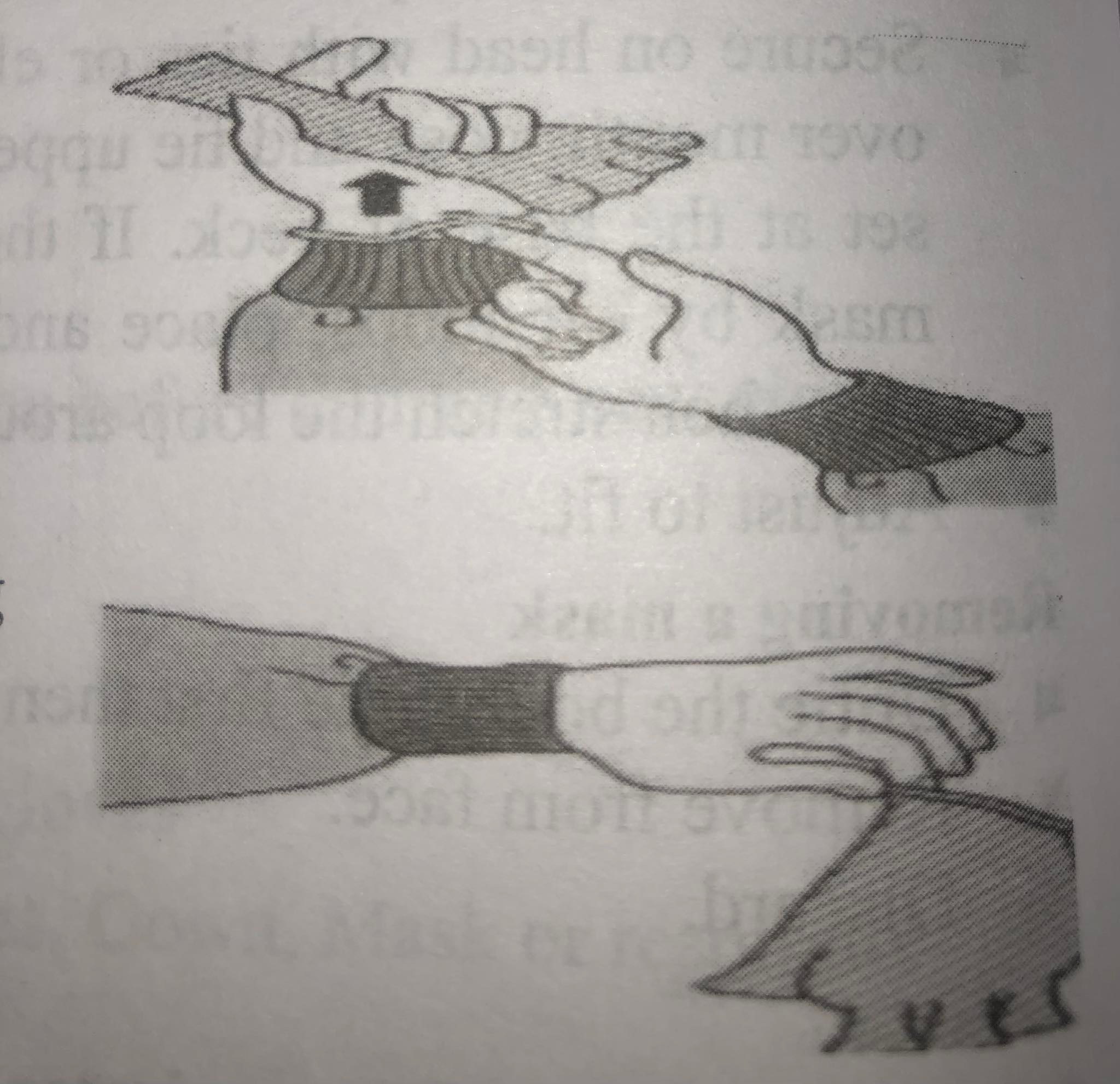
- Place the mask over nose, mouth and chin. Determine which side of mask is in top and front.
- Fit flexible nose piece over Nose Bridge.
- Secure on head with ties or elastic. If mask has ties, place mask over mouth, nose and tie upper set at the back of head and lower set at the base of neck. If the mask has elastic ear loops, hold mask by ear loops, place and hold mask over nose, mouth and chin then stretch the loop around each ear.
- Adjust to fit.
Removing a Mask
- Untie the bottom tie first then top tie.
- Remove from face.
- Discard.
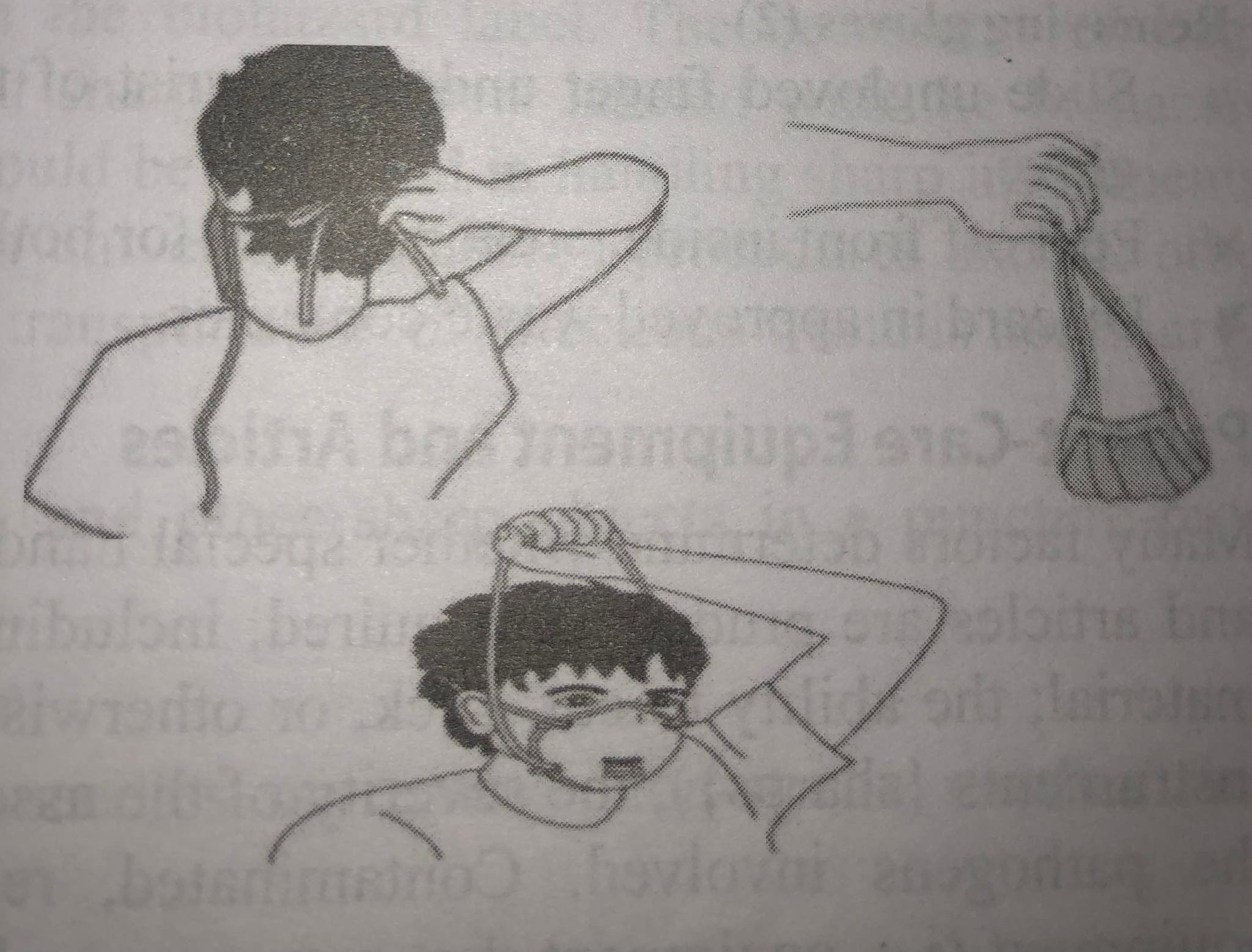
Removing a Particulate Respirator
- Lift the bottom elastic over your head first.
- Then lift off the top elastic.
- Discard.
Goggles/Protective Eye Wear
Eye goggles or glasses and face shields provide barrier protection against splashes and sprays.
How to don eye and face protection
- Position goggles over eyes and secure to the head using the ear pieces or headband.
- Position face shield over face and secure on brow with headband.bun
- Adjust to fit comfortably.
Remove Goggles or Face Shield
- Grasp ear or head pieces with ungloved hands.
- Lift away from face.
- Place in designated receptacle for reprocessing or disposal.
Gloves
Gloves are clean or sterile fitted coverings for the hands, usually with a separate sheath for each finger and thumb which are worn during medical examinations and procedures. Gloves can be used as a physical barrier to interrupt transmission and to avoid direct contact with infectious material.
Donning Sterile Gloves
- Wash hands.
- Select correct type and size.
- Open the outer glove package.
- Use one hand to grasp the inside upper surface of the gloves cuff for the opposite hand, lift the glove up and clear it of the wrapper.
- Insert opposite hand into gloves, placing thumb and finger into proper openings.
- Pull gloves into place, touching only the inside of glove at cuff. Leave cuff in place.
- Slip the fingers of the sterile gloved hand inside the cuff of remaining glove while keeping the thumb pointed outward. of Tavo apm
- Insert the ungloved hand into the glove. Pull the second glove on, touching only the outside of the sterile glove with the other sterile gloved hand and keeping fingers inside the cuff.
- Extend gloves over isolation gown cuffs.
Removing Gloves (1)
- Grasp outside edge near wrist.
- Peel away from hand, turning glove inside-out.
- Hold in opposite gloved hand.
Removing Gloves (2)
- Slide ungloved finger under the wrist of the remaining glove.
- Peel off from inside, creating a bag for both gloves.
- Discard in approved waste container.
Patient-Care Equipment and Articles
Many factors determine whether special handling and disposal of used patient-care equipment and articles are prudent or required, including the likelihood of contamination with infective material; the ability to cut, stick, or otherwise cause injury (needles, scalpels, and other sharp instruments {sharps}); the severity of the associated disease; and the environmental stability of the pathogens involved. Contaminated, reusable critical medical devices or patient-care equipment (i.e. equipment that enters normally sterile tissue or through which blood flows) or semi critical medical devices or patient-care equipment (i.e., equipment that touches mucous membranes) are sterilized or disinfected (reprocessed) after use to reduce the risk of transmission of microorganisms to other patients; the type of reprocessing is determined by the article and its intended use, the manufacturer's recommendations, hospital policy, and any applicable guidelines and regulations.
Noncritical equipment (i.e. equipment that touches intact skin) contaminated with blood, body fluids, secretions, or excretions is cleaned and disinfected after use, according to hospital policy. Contaminated disposable (single-use) patient-care equipment is handled and transported in a manner that reduces the risk of transmission of microorganisms and decreases environmental contamination in the hospital; the equipment is disposed of according to hospital policy and applicable regulations.
Safe Waste Handling and Disposal of Infectious Waste and Sharp Objects
Infectious waste has epidemiologic evidence which is capable of transmitting a dangerous communicable disease. WHO defines infectious waste as "waste contaminated with blood and its byproducts, cultures and stocks of infectious agents, waste from patients in isolation wards, discarded diagnostic samples containing blood and body fluids, and contaminated materials (swabs and bandages) and equipment (such as disposable medical devices)." Infectious waste includes liquid blood or regulated body fluids from humans or research animals, wastes that will release blood or regulated body fluids, contaminated sharps from human or any animal use, live or attenuated human and zoonotic vaccines and contaminated laboratory items. Staffs handling infectious waste should wear personal protective equipment as necessary. Contaminated sharps are any contaminated or potentially contaminated items from human or animal care that can induce sub-dermal inoculation, including needles, scalpel blades, pipettes, lancets, and glass or rigid vials that contained infectious agents. Needle-stick injuries are wounds caused by needles that accidentally puncture the skin. Injection of blood-borne viruses is the major hazard of needle stick injuries, especially the viruses that cause AIDS (the HIV virus), hepatitis B and hepatitis.
Patient-care equipment should be handled in a manner that prevents personal skin and mucous membrane exposure and cross contamination to other patients. Safe Picking up and transporting infectious waste is very important. cleaned, disinfected and sterilized before using it in the care of another patient. Disposal single use instruments should be used as far as possible. At all times prior to disposal, infectious Reusable equipment must be thoroughly waste should be stored in closed containers in a secure area, protected from adverse environmental conditions and identified with the biohazard label. The necessary red bags and/or leak-proof, rigid and puncture resistant sharps containers labeled with the biohazard symbol should be used. Safety precautions should be practiced in handling sharp instruments. Providing necessary instruction and training in universal precaution procedures and all other applicable guidelines regarding the handling or transportation of infectious waste is necessary.
Safe Disposal of Sharp Objects/Needle
- Place all needles, syringes, scalpel blades, and other sharp objects in a puncture-proof container.
- Secure sharps with a magnet when applicable.
- Put needles into cork and do not re-cap needles or remove non-sterile needles from disposable syringes.
- Do not attempt to bend of break a needle before discarding.
- Store a sharp waste container near where the sharps are generated.
- Immediately discard sharps after use.
- Sharp containers must be placed at the work sites.
Recognizing a Sharps Container
A sharps container is a receptacle intended for the collection and disposal of sharps. It is rigid- walled, puncture-proof and sealable. Following are features of sharp container: yellow in colour, labelled as "sharps" or "infectious waste" and carries the biohazard symbols.
Housekeeping and Management of Spillage
Housekeeping service in a hospital has a major role in minimizing the hospital acquired infections to the patients and to reduce the medical costs for the patient. Housekeeping activity in any hospital provides a clean, hygiene and safe environment for patients and general public. Housekeeping comprises of various activities like maintenance of beds in wards, rooms, operation theatres and outpatient departments.
Objectives
- Establish a welcoming atmosphere and a well-mannered, reliable service from staff of all departments.
- Make sure a high standard of cleanliness and general maintenance in all areas.
- Provide the maximum care and comfort to the patients
Responsibilities
- Develop guideline for appropriate cleaning techniques, procedure, frequency, agents used and waste management.
- Inform to the maintenance service of any building problems requiring repair: cracks, defects in the sanitary or electrical equipment, etc.
- Classify the different hospital areas by varying need for cleaning (High risk/Medium risk/Low risk area).
- Continue supervision and monitoring.
Selection of disinfectant for surface cleaning
- Liquid soap/ detergent,
- Chlorine solution,
- Phenol,
- Alcohol,
- Hypochloride, etc.
Care of Environment
Each hospital, clinic should have procedures for care, cleaning, and disinfection of environmental surfaces. Spills of blood or body fluids need to be handled with special procedures.
The room, or cubicle, and bedside equipment of patients on Transmission-Based Precautions are cleaned using the same procedures used for patients on Standard Precautions, unless the infecting microorganism(s) and the amount of environmental contamination indicate special cleaning. In addition to thorough cleaning, adequate disinfection of bedside equipment and environmental surfaces (e.g. bed rails, bedside tables, carts, commodes, doorknobs, faucet handles) is indicated for certain pathogens, especially enterococci, which can survive in the inanimate environment for prolonged periods of time. Patients admitted to hospital rooms that previously were occupied by patients infected or colonized with such pathogens are at increased risk of infection from contaminated environmental surfaces and bedside equipment if they have not been cleaned and disinfected adequately. The methods, thoroughness, and frequency of cleaning and the products used are determined by hospital policy.
Management of Spillage
The factors involved in spill management are:
- The nature of the spill e.g. Sputum, vomit, faeces, urine, blood.
- The size of the spill (e.g. Spot [few drops], small [<10cm] or large [>10cm])
- Volume of spill (less than 30 ml, more than 30 ml)
- The type of surface: Carpet or floor.
Procedure for Spill Management
- Wear Personal Protective Equipment (PPE).
- Spray 0.5% chlorine and Cover the area with paper towel/cloth sock the spillage.
- Leave it for 15 minutes.
- Wipe and discard contaminated paper towel/cloth in disposable bag.
- Mop the spillage using disposable cloth or wipes until the area is visibly clean.
- Remove the gloves and discard in the same bag, tie the bag properly and put label with the type of spillage.
- Wash the hands properly with soap and water.
- Fill incident form and submit.
Laundry Services
Laundry Services A laundry service is responsible for providing an adequate, clean and constant supply of linen to respective departments. Although soiled linen may be contaminated with pathogenic microorganisms, the risk of disease transmission is negligible if it is handled, transported, and laundered in a manner that avoids transfer of microorganisms to patients, personnel, and environments. The methods for handling, transporting, and laundering of soiled linen are determined by hospital policy and any applicable regulations.
Functions of laundry department
- Collect or receiving soiled and infected linen.
- Sorting the linen and process them.
- Inspect and repair or replacing damaged material.
- Distribute clean linen to the respective wards.
- Maintain different types of registers.
Collecting, Transporting and Sorting Soiled Linen
- Handled in a way to prevent contamination of skin, mucous membranes, and clothing. Use personal protective equipment while collecting and transporting linen
- Collect and remove soiled linen after each procedure or patient bed. Do not sort and wash patient care area.
- Fold soiled linen with contaminated area to the inside.
- Hold away from body and place in appropriate bag and dispose of properly in leakage resistant bags. Use double bagged when transporting linen.
- Transport soliled and clean linen separately and labeled accordingly.
- Wash hands after collection.
Washing and Drying
- Decontamination if infected.
- Wash thoroughly and separately with warm water.
- Completely dry the linen.
- Check holes and should be ironed.
- Always clean washing areas.
Care of Linen Materials
- Using large amount of washing soda and bleaching agent can damage the linen.
- Rinse the fabrics properly to avoid deposition of detergents.
- The materials should be dried up properly otherwise it generate, terrible odor and so the lifetime of the materials will be shortened.
- Linen materials should be stored in dry places.
Storing, Transportation and Distribution
- Store, clean linen in clean, closed storage areas.
- Distributing cart should be cleaned before placing the clean linen.
- Clean linen must be wrapped or covered during transport.
Surgical Asepsis
Surgical Asepsis is the absence of all microorganisms within any type of invasive procedure. Sterile technique is a set of specific practices and procedures performed to make of micro-organisms is termed sterile. For example, a tear in a surgical gloves expose the outside of the glove to the skin surface, thus contaminates it. Principles of sterile technique help control and prevent infection, prevent the transmission of all microorganisms in a given area, and include all techniques that are practiced to maintain sterility.
Sterile technique is most commonly practised in operating rooms, labour and delivery rooms, and special procedures or diagnostic areas. It is also used when performing a sterile procedure at the bedside, such as inserting devices into sterile areas of the body or cavities e.g. insertion of chest tube, central venous line, or indwelling urinary catheter. In health care, sterile technique is always used when the integrity of the skin is accessed, impaired, or broken e.g. burns or surgical incisions. Sterile technique may include the use of sterile equipment, sterile gowns, and gloves.
Sterile technique is essential to help prevent surgical site infections (SSI), an unintended and oftentimes preventable complication arising from surgery. SSI is defined as an "infection that occurs after surgery in the area of surgery". Preventing and reducing SSI are the most important reasons for using sterile technique during invasive procedures and surgeries. Implementing Surgical Asepsis includes:
- Creation of a sterile environment,
- Use of sterile equipment/supplies,
- Sterilization of reusable supplies,
- Surgical hand scrub,
- Surgical attire,
- Sterile gloves,
- Sterile field,
- Use of sterile technique.
Difference between Medical and surgical Asepsis
| Medical Asepsis | Surgical Asepsis |
|
|
|
|
|
|
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google