Planning
Subject: Fundamentals of Nursing

Overview
Planning is the term used to describe a complete plan created by a nurse that starts with the first patient interaction and lasts until the patient is discharged from the health agency. It is the decision-making phase in the nursing process. A nursing action plan should be created to help the patient resolve his condition once the patient and nurse have reached an understanding regarding the diagnosis. The patient should be included in the process of creating the strategy, and his preferences should be considered as much as is practical.
Purposes
- To achieve a greater level of performance and wellness.
- To determine if the client's health has changed in any way. (Repeated Planning)
- Maintain the patient's present level of health and functionality (in case of potential problems.)
- To adapt to a lesser level of health and functioning when a treatment is not possible.
- Should have a plan in place in case a patient develops a fatal illness and their life is in risk.
Types of Planning
Initial planning: The nurse who conducts the admission evaluation typically develops the initial comprehensive plan of care. The client's body language is visible to the nurse, and she also has access to certain intuitive knowledge that would not otherwise be available. Standardized care plans specify the nursing diagnoses and supporting therapies. The nurse performing the admission, nursing history, and physical assessment should start making plans as soon as feasible due to the trend toward shorter hospital stays.
Ongoing planning: Every nurse who interacts with a patient is in charge of continual planning. Nurses can further customize the initial care plan as they gather more details and monitor the client's response to treatment. In addition, the nurse plans the care that will be given that day as part of ongoing planning at the beginning of a shift. The nurse performs daily planning for the following objectives using data from ongoing assessments:
- To see if the client's health state has changed.
- To establish priorities for the client's care throughout the shift.
Discharge planning: This is the procedure for foreseeing and making plans for post-discharge requirements. Due to the usual length of stay of clients, who are occasionally discharged while still needing care, it is a crucial component of comprehensive health care and should be addressed in each client's care plan. Such care is increasingly provided in the home, even if many clients are discharged to other organizations (such nursing homes).
Steps of planning
- Setting priorities
- Writing nursing goals
- Planning nursing actions
Setting Priorities
Prioritization refers to the process of ranking nursing diagnoses or patient problems in order of priority and urgency in order to establish a preferred sequence for nursing interventions. It comprises ranking the nursing issues or choosing which of the issues that have been identified requires immediate attention and which can wait. When a patient has numerous diagnoses and associated concerns, priorities help in anticipating and timing nurse intervention. Diagnoses made by nurses are given a high, medium, or low priority.
- High priority nursing diagnoses: High-priority nursing diagnoses are ones that are life-threatening and must be addressed immediately. Priority is given to nursing diagnoses that, if left untreated, could cause harm to a patient or others. High-priority nursing diagnoses include "high risk for aspiration," "high risk for violence- self-directed or directed at others," "impaired gas exchange," and "decreased cardiac output." In an emergency or critical care setting, people can develop multiple high-priority nursing diagnoses at the same time.
- Intermediate priority: These are non-emergency and non-life threatening conditions such as altered bowel habits, impaired skin integrity, knowledge deficits, and decreased mobility.
- Low priority: Nursing with a low priority The patient's well-being is affected by a diagnosis that is not necessarily directly tied to a specific condition or prognosis. i.e. altered sleep pattern, risk of chronic respiratory infections due to a 20-year smoking history
Prioritization may be conducted to:
- Determine which health condition to address first based on the critical need determined by a review of available data.
- Prepare a plan for addressing health needs based on the resources available.
- Determine which health conditions are most likely to be impacted successfully by accessible evidence-based therapies.
The following points should be considered while setting priority.
- Make use of Maslow's hierarchy of requirements.
- Consider the urgency of his/her concerns, such as hemorrhage, breathing difficulty, and so on.
- When possible, consider the client's priorities.
- Consider the client's health ideals and beliefs.
- Priority setting includes ethical care. When ethical considerations cloud priorities, it is critical to have open communication with the patient, family, and other health care providers.
- Consider the availability of time and resources, such as time, cost, person, and equipment.
- Priorities shift as a patient's condition changes, sometimes in a matter of minutes.
- Consider the patient's potential impact of future issues.
- Medical treatment strategy
Writing Nursing Goal
The nurse should list the nursing goal for each issue after ranking the patient's worries in order of importance. It also acts as a schedule for the test. A goal is a broad declaration that identifies intended changes in a patient's condition or behavior. In order for the nurse and client to evaluate the client's progress toward the desired objectives as well as the effectiveness of nursing intervention, the goals must also be measurable and realistic. A goal is to lessen or completely eradicate the challenges identified in the patient's assessment. Depending on how long it takes to accomplish a goal, it might be long-term or short-term.
- Short term goals: When the goals are likely to be achieved fairly e.g. within few hours or days they are called short term goals.
- Long term goals: When the goals are likely to take many days or months to achieve, they are considered to be long-term goals.
Goals are essential for the nursing-care plan because a goal gives direction to the nursing intervention.
- Serves as a guide for nursing action
- Motivates the patient as well as the nurse to continue their effort.
- Serves as a criterion to evaluate the effectiveness or nursing intervention.
Guidelines for Writing Goals
Goals should be:
- Related to the trauma response.
- Client-centered.
- Address what the client will do, when and what extent it will be accomplished.
- Clear and concise. Ambiguous of abstract wording should be avoided.
- Observable and measurable
- Time limited.
- Realistic.
- Determined by client and nurse together
- Specific.
- Assignable- specify who will do it.
- Achievable
- Relevant
An expected outcome is a quantifiable shift in a patient's condition that you anticipate happening as a result of nursing care or a metric to gauge goal achievement. For a single aim, there may be multiple expected outcomes that must be achieved. Additionally, a list of the desired outcomes broken down into steps might help you organize actions in a practical way. Always include time frames and a chronological list of expected results.
Planning Nursing Action
Nursing actions are particular nursing tasks that are intended to carry out in order to accomplish the objective. After nursing diagnoses are determined and goals and outcomes are chosen, you decide on an intervention tailored to the patient's circumstances. When deciding on nursing interventions, the patient should be consulted. When planning nursing interventions, the following factors should be taken into account:
- The planned nursing action must be safe for the patient.
- It must be realistic.
- It must be based on scientific principles.
- It must accomplish the stated goal.
Types of nursing interventions:
- Independent interventions: activities that are nurses are licensed to initiate e.g.: back care, catherization, counseling, health teaching, emotional support etc.
- Dependent interventions: activities carried out under physicians order eg: medication, diagnostic procedure etc.
- Collaborative interventions: activities carried out in collaboration with other health team members such as: physiotherapy, nutrition therapy etc.
After choosing appropriate nursing interventions the nurse writes those on the plan on nursing orders. Choosing suitable nursing interventions involves critical thinking and your ability to be competent in three areas:
- Knowing the scientific rationale for the intervention
- Possessing the necessary psychomotor and interpersonal skills
- Being able to function within a particular setting to use the available health care resources effectively.
Components of nursing order
| Date | action verb | content area | Time allocated | signature |
| 2075/10/10 | change | client's position | 2 hourly |
Implementation
The fourth step in the nursing process is this. officially starts once the nurse creates a plan of care based on a precise and pertinent nursing diagnosis. The nurse then launches interventions that are intended to achieve the targets and anticipated results required to maintain or enhance the patients' health state. A nursing intervention is any procedure carried out by a nurse to improve patient outcomes that is supported by clinical judgment and expertise. The stated goal is what implementation tries to achieve. In order to ensure continuity of care for the patient during hospitalization and in the lead-up to discharge, nursing care is provided in accordance with the care plan.The solutions a nurse employs should ideally be evidence-based, offering the most recent, cutting-edge, and efficient techniques to managing patient concerns. Implementation may take hours, days, weeks, or even months to complete. Before, during, and after interventions, the nurse must continue to evaluate the client's condition. The nurse receives baseline information from the assessment before the intervention. The nurse can gauge the client's reaction—whether good or negative—through assessment before, during, and after the intervention. The nurse must take necessary measures if there are bad reactions while doing the procedure. If there are favorable results, the nurse enters this data into the database to assess the effectiveness of the intervention.
To carry out the intended nursing interventions, the nurse must also have psychomotor abilities, interpersonal skills, and critical thinking abilities. Even if the planning is done correctly, there are various variables that could emerge and prevent the plan from being implemented. The nurse should be adaptable when delivering the care. For instance, it could be challenging to carry out the care according to the plan if the equipment isn't ready, the doctor is on his rounds, visitors show up, or the patient experiences another emergency. Interventions consist of both direct and indirect care methods for people, families, and the community.
- Direct care: Direct care interventions are treatment performed through interactions with patients. For example, a patient receives direct intervention in the form of medication administration, insertion of intravenous infusion and counseling during a time of grief.
- Indirect care: Interventions are treatments performed away from patient but on behalf of the patient or group of patients. For example, indirect care measures include actions for managing the patient's environment eg. Safety and infection control, and documentation.
Use critical thinking to determine whether a planned intervention is still appropriate for the patient's clinical state before putting it into action. Always pause before acting. The circumstances of patients frequently vary minute by minute. You must take into account the nursing unit's activity schedule, which frequently determines when and how to conduct an intervention. Your choices regarding whether and how to intervene are influenced by a variety of circumstances. It is your responsibility to possess the knowledge and clinical proficiency required to carry out interventions for your patients in a safe and efficient manner. Following are some suggestions for making decisions during implementation:
- Review the set of all possible nursing interventions for the patient's problem.
- Review all possible consequences associated with each possible nursing action.
- Determine the probability of all possible consequences.
- Make a judgment of the value of the consequence to the patient
When implementing interventions, nurses should follow these guidelines:
- Based nursing interventions on scientific knowledge, nursing research, and professional standards of care whenever possible.
- Clearly understand the order to be implemented and questions any that are not understood.
- Adapt activities to the individual client, a client's beliefs, values; age, health status, and environment are factors that can affect the success of a nursing action.
- Implement safe care.
- Provide teaching, support and comfort to enhance the effectiveness of nursing care plans.
- Be holistic; view the client as a whole.
- Respect the dignity of the client and enhance the client's self-esteem.
- Encourage the client to participate actively in implementing the nursing interventions.
- Documenting Nursing Activities.
Process of Implementation
The process of implementation normally includes:
- Assessing or reassessing the client:
- Assessment is a continuous process that occurs each time you interact with a patient. While providing care, nurses must continue to collect data about changes in the patient's level of wellness, health problems as well as reactions, feelings and strengths. Reassessment often focuses on one primary nursing diagnosis, or one dimension of the patient such as level of comfort, or one system such as the cardiopulmonary system. The reassessment helps to decide if the proposed nursing actions are still appropriate for the patient's level of wellness.
- Reviewing and revising the existing nursing care plan:
- After the reassessing the patient, review the care plan and compare assessment data to validate the nursing diagnosis and determine whether the nursing interventions remain the most appropriate for the clinical situation. If the patient's status has changed and the nursing diagnosis interventions are no longer appropriate, modify the nursing care plan.
- Organizing resources and care delivery:
- The resources of the facility include equipment and skilled personnel. Organization of equipment and personnel makes timely, efficient, skilled patient care possible. It is also important to prepare the environment and patient for a nursing intervention. Before performing an intervention, decide which supplies you need and determine their availability. Always place equipment in a convenient location to provide easy access during a procedure. As a nurse you are responsible for deciding whether to perform an intervention or delegate it to another member of the nursing team. When the intervention are complex or physically difficult probably need assistance from co colleagues or patients family. The patient care environment needs to be safe and conductive to implementing therapies.
Determining the nurse's need for assistance: When implementing nursing strategies, the nurse may require assistance for one of the following reasons:
- If the nurse is unable to implement the nursing strategies safely alone for one example turning an obese patient in bed.
- The nurses also need assistance if they lack the knowledge or skills to implement any particular nursing activity.
Implementing nursing intervention:
To assist the client in achieving his or her health goals, nursing strategies are put into practice. Nursing tasks can be performed independently, with another person, or in a group. Implementing nursing strategies should take into account the following:
- The client in individual.
- The client's need for involvement.
- Prevention of complication.
- Preservation of the body defenses.
- Provision of comfort and support to the patient
- Accurate and careful implementation of all nursing activities.
Documenting nursing activities:
Nursing action plans and care guidelines are frequently presented verbally as well as in writing. By documenting the interventions and the client's reactions in the nurse's notes, the nurse completes the implementing phase. The senior nurse or the doctor may want to stay up to speed with verbal reports regarding the patient when their health is changing quickly. At the conclusion of the shift, the nurse may enter recurring or routine tasks in the client's record. In nursing, immediate recording is crucial.
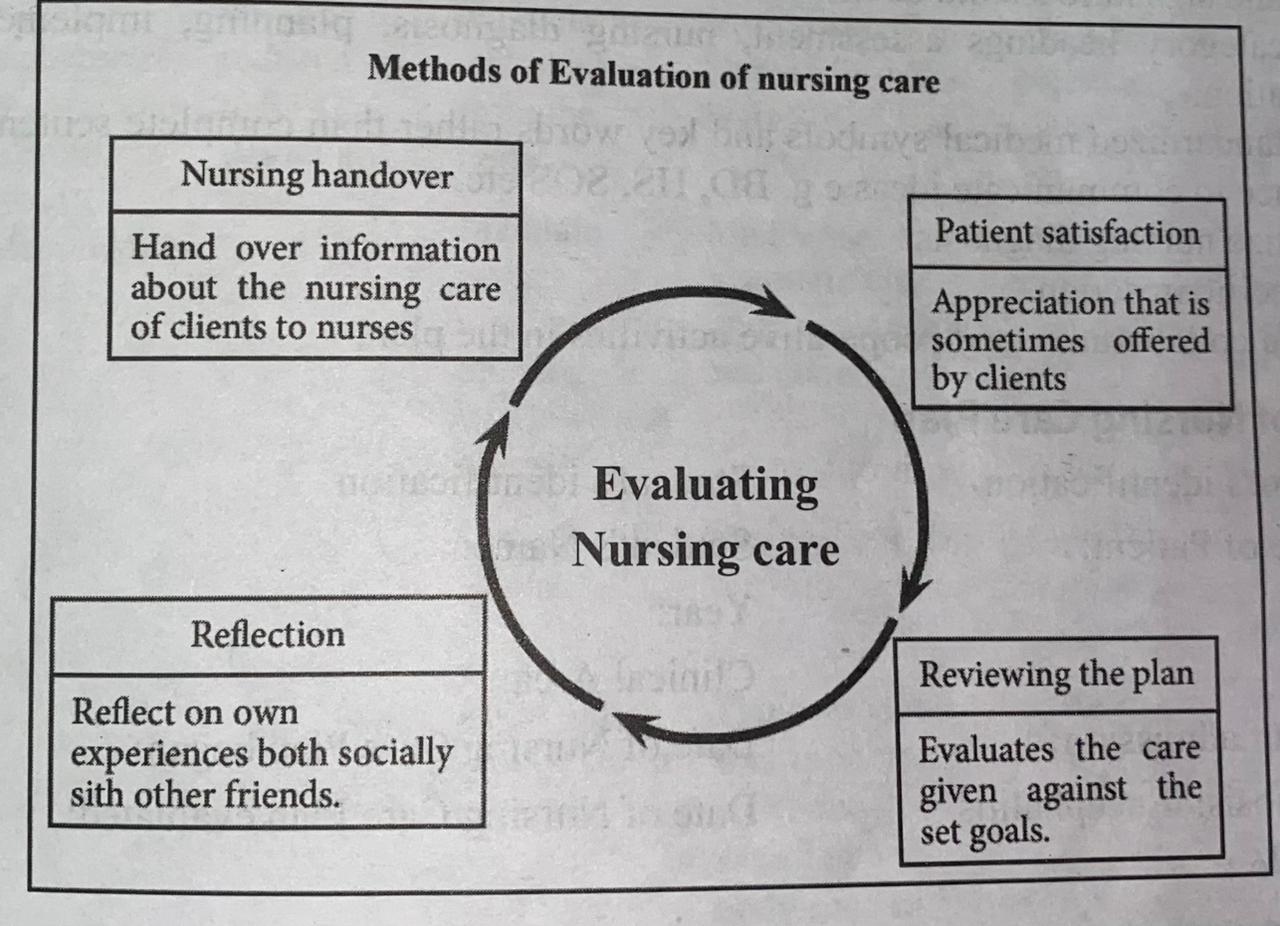
Evaluation
The fifth step in the nursing process is evaluation. Based on the client's behavioral responses, nursing care effectiveness is assessed in relation to the client's goals. It's a continuous process. The nurse conducts an assessment to establish whether the objectives for the patient's wellbeing have been fulfilled after all nursing interventions have been carried out. In order to make wise decisions at subsequent stages of the nursing process, nurses regularly examine data. The care plan must be continually assessed for both the patient's condition and the nursing staff's efficacy. It is a crucial part of discharge planning because it enables the nurse to consult with patients and families to determine whether more medical attention is required, and then to make the appropriate referrals.
Purposes
The purposes of evaluation as described by the Open University publication (1984) are:
- To determine whether patient's goals/expected outcomes have been achieved.
- To measure standards of nursing care.
- To measure the quality of nursing care.
- To discover which nursing actions are most consistently effective in solving a particular patient problem.
- To measure staff performance.
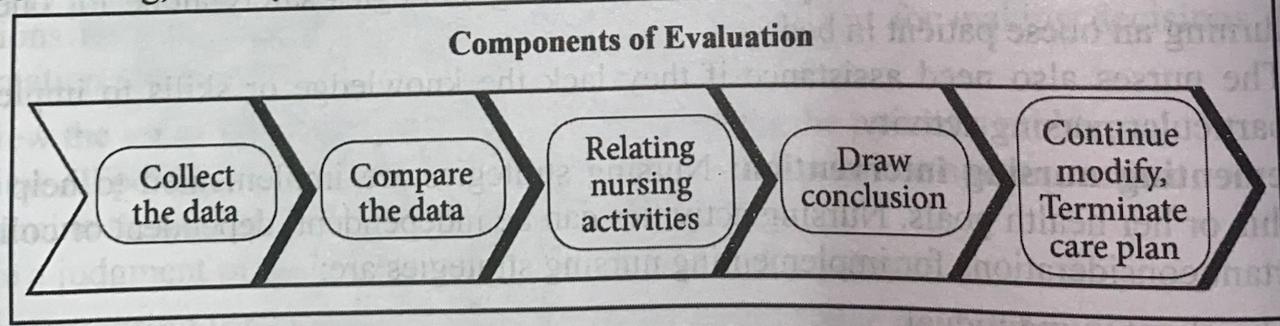
Process of evaluating client responses
- Collecting data related to the desired outcomes.
- Compering the data with outcomes
- Relating nursing activities to outcomes
- Drawing conclusions about problem status
- Continuing, modifying or terminating the nursing care plan.
The possible patient outcomes are generally described under three terms: patient's condition improved, patient's condition stabilized, and patient's condition deteriorated, died, or discharged. It involves determining whether client's goals have been met, partially met or not met.
- Goal met: if the patient is able to demonstrate the behavior within the date and time specified in the goal statement, the goal is met
- Goal partially met: if the patient is able to demonstrate the behavior but not at the extent the nurse had specified in the goal statement, the goal is partially met.
- Goal not met: if patient is unable or unwilling to perform the behavior at all, the goal is not met.
If the goal has been met, the nurse must then decide whether nursing activities will cease or continue in order for the client's status to be maintained. If the goal has been partially met or not been met, the nurse must reassess the situation. for example:
Goal- Pain will be relieved within 1/2 an hour after administration of pain relieving medicine.
Evaluation- Done after 1/2 an hour of administration of pain relieving medicine.
- Pain was relieved - Goal was achieved.
- Pain was slightly reduced - Goal was partially achieved.
- Pain was not at all reduced - Goal was not achieved.
Data are collected to determine why the goal has not been achieved and what modifications to the plan of care are necessary. There are a number of possible reasons that goals are not met or are only partially met, including.
- The initial assessment data were incomplete.
- The goals and expected outcomes were unrealistic.
- The time frame was too optimistic.
- The goals and nursing interventions planned were not appropriate for the specific clients.
Nursing Care Plan
A nursing care plan is a documented plan or directive for nursing action (activities), developed in response to an evaluation of changes in the patient's health status. Priorities, goals, planning, nursing interventions, reasoning, and evaluation are all included in the nursing diagnosis. The final step of the planning phase is the creation of the nursing care plan. The full care plan serves as a blueprint for nursing action, offering guidance for carrying it out and a framework for assessing the client's reaction to nursing action.
Purpose of the Written Care Plan
- Care plans provide direction for individualized care of the client. A care plan flows from each patient's unique list of diagnoses and should be organized by the individual's specific needs.
- Continuity of care. The care plan is a means of communicating and organizing the actions of a constantly changing nursing staff. As the patient's needs are attended to, the updated plan is passed on to the nursing staff at shift change and during nursing rounds.
- Care plans help keep documentation. The care plan should specifically outline which Pre observations to make, what nursing actions to carry out, and what instructions the client or Poss family members require.
- They serve as a guide for assigning staff to care for the client. There may be aspects of the 01 patient's care that need to be assigned to team members with specific skills.
- Care plans serve as a guide for reimbursement. Medicare and medicaid originally set the plan in action, and other third-party insurers followed suit. The medical record is used by the insurance companies to determine what they will pay in relation to the hospital care received by the client. If nursing care is not documented precisely in the care plan, there is no proof the care was provided. Insurers will not pay for what is not documented.
Guidelines for writing Nursing care plans
- Date and signature should be mention.
- Use category headings assessment, nursing diagnosis, planning, implementation and evaluation.
- Use standardized medical symbols and key words rather than complete sentence complete sentence to communicate ideas e.g. BD, HS, SOS etc.
- Prioritize nursing diagnosis
- Be specific in action.
- Include collaborative and cooperative activities in the plan.
Example of Nursing Care Plan
Patient's identification Student's identification
Name of Patient: Student's Name:
Age: Year:
Sex: Clinical Area:
Date of admission: Date of Nursing Care Plan began:
Diagnosis: Encephalitis Date of Nursing Care Plan evaluated:
Bed No.:
Patient's assessment
16 years, Mr. Ram was admitted in medical ward yesterday with the two days history of unconsciousness. Now he is still unconscious. Can't move his body himself, smelly secretion + + in mouth, oral care has not given for 3 days. Intravenous fluids 5%, dextrose 8 hourly going on, can't eat himself, has not passed stool for 3 days, decrease bowel sound on auscultation, temperature 39°C, dirty body and hair.
Patient's health problems
- Temperature 39°C
- Can't turn his body himself
- Smelly secretion + in mouth
- Can't eat himself
- Constipation
- Dirty body and hair
Actual nursing diagnosis
- Alteration in body temperature, 390c related to inflammation of brain tissue.
- Poor oral hygiene related to inability to take care himself.
- Poor personal hygiene: dirty hair and body related to inability to take care himself.
- Alteration in elimination: constipation related to immobility.
Potential nursing diagnosis
- Risk of nutritional deficit related to lack of intake.
- Risk of pressure sore related to immobility.
- Risk of oral infection related to lack of oral care.
- Risk of urinary tract infection related to indwelling catheter.
- Risk of joint contracture related to immobility of joints.
|
s. N |
Date |
Nursing Diagnosis |
Nursing Goal |
Planning | Implementation | Rational | Evaluation |
| 1 | Alteration in body 39 C related to brain tissue inflammation | Temperature will be to 37 C within an hour | Removed all extra clothes and blanket from the body | Removed all extra clothes and blanket from the body | Heat loss through radiation | Goal was fully achieved as the temperature decreased upto 37°C after giving tapid sponge after 50 minutes. | |
| Maintained cross ventilation by opening windows and doors. | Maintain cross ventilation by opening windows and doors. | Heat loss through convection | |||||
| Open fan if available. | Fan was opened. | Heat loss through convection | |||||
| Apply tapid sponge for 20 minutes. | Tapid sponges was applied for 20 minutes in varied site of body such as forehead, axilla, etc. | Heat loss through conduction | |||||
|
Give antipyretic medicine (Paracetamol 500 mg). According to doctor's order. If above measure failed. |
Provided antipyretic medicine (paracetamol 500mg) | Acts on temperature regulating centres (hypothalamus) | |||||
| Encourage to drink oral fluid. | Encouraged to drink oral fluid. | Replaces fluid loss. |
Pre and post-operative nursing care plan
Possible pre-operative nursing diagnosis
- Fear related to surgery/unknown cause.
- Anxiety related to knowledge deficit/effect of surgery on ability to function.
- Post-operative nursing diagnosis.
- Ineffective airway clearance related to anaesthesia.
- Ineffective breathing pattern related to pain, general anaesthesia and decreased energy.
- Pain related to surgical incision.
- Hypothermia related to exposure to cool environment.
- High risk for altered urinary elimination related to decrease bladder tone secondary to effect of general anesthesia.
- Potential for wound infection related to surgical incision.
- Risk of chest infection related to anesthesia and immobility.
- Potential for constipation related to surgical manipulation of intestine, pain medication and immobility.
- Potential altered nutrition: less than body requirements related to nausea and diminished peristalsis.
- Knowledge deficit follow-up care and home care related to change in health status
|
S N |
Date |
Nursing diagnosis |
Nursing Goal | planning | Implementation | rational | evaluation |
| 1 | Pain related to surgical incision | patient states relief of pain to tolerable level or pain will be reduced up to tolerable level within 1/2 an hour | Determined location, duration, intensity and possible causes of pain before administering the medication. | Determined location, duration, intensity and possible causes of pain before administering the medication. | cause of pain must be identified. it is unsafe to assume all post-operative pain related to surgery | goal was achieved as patient states relief of pain. After 1/2 am Hour. | |
| 2 | Give analgesic at prescribed interval (e.g. morphine 5mg Im) and also encourage the patient to request analgesic before pain becomes severe. | provide analgesic at prescribed interval (e.g. morphine 5mg Im) and also encourage the patient to request analgesic before pain becomes severe. | Administration of analgesic before pain becomes severe maintains better pain control. Adequate pain management promotes patient participation in post-operative activities. | ||||
| 3 |
Provide non- pharmacologica 1 pain relief measures to augment analgesic such as: Comfortable position Position change |
Provide non- pharmacologica 1 pain relief measures to augment analgesic such as: Comfortable position Position |
These measures promote relaxation and enhance pain relief. Not all discomfort or potential problem related to surgery is incisional. These measures can be utilized by family as well. | ||||
|
change distraction smooth bedding back rub or massage |
change distraction smooth bedding back rub or massage |
||||||
| 4 |
Assessed the effectiveness of pain relief. Such as: Ask the patient whether the pain is relieved to tolerable level. Monitor nonverbal signs of pain relief. Assess vital signs |
Assessed the effectiveness of pain relief. Such as: Ask the patient whether the pain is relieved to tolerable level. Monitor nonverbal signs of pain relief. Assess vital signs |
evaluates effectiveness of pain management |
Method of Physical Examination
Equipment Required for the Physical Examination
- Screen
- Weight machine.
- Top sheet/ blanket to cover the patient during examination.
- Dress for patient
- A tray containing
- Paper bag with cotton swab
- Vitals sign tray including Sphygmomanometer, Stethoscope, Thermometer and Tape measure
- Flashlight
- Lubricating jelly
- Oto-ophthalmoscope
- Tissues
- Paper towels
- Tongue depressors
- Pocket eye chart
- Tuning fork (128 Hz)
- Rectal gloves
- Reflex hammer
Procedure for Doing a Physical Examination
- Explaining the purposes and procedure for physical examination.
- Wash hands
- Prepare the patient for physical examination.
- Take clinical measurements like height, weight and vital signs.
- Tell the patient how long the examination will take.
- Asking him to urinate.
- Arranging for a quiet, private area for assessment.
- Asking the patient to remove his clothes and giving him a drape to cover.
- Inspect the patient's general appearance.
- Assess the physical status of the patient in a systematic way by using various methods of physical examination.
- After completing the physical examination, allow the patient to put on his clothes.
- Wash hands.
- Explain the findings to the patient.
- Record the relevant findings of physical examination on the patient's assessment form.
Positioning
- Have the client seated as you begin the examination
- If the client is unable to sit, use fowler's or semi flower's position.
Steps of Doing a Physical Examination
- Measurement:
- Take Height, weight and vital signs.
- General appearance:
- Use inspection and observe the behaviour
| Examination | Normal data | Abnormal data |
| Assess overall body apperance and mental status | Normal apperance | |
| Observe the client level of consciousness and orientation | Oriented to time place and person | Disorientated |
| Observe facial expression and mode | Cheerful and stable mood | |
| Gait | Walks straight | Limps |
| General state of health | Cheerful, active and appears healthy | Sad,tired,weak appearance |
| Stature: Note the general bodily proportions and look for any deformities. | Normal weight and height for age | Very short stature in turner's syndrome, renal disease, hypopituitary (Dwarfism), long limbs in marfan's syndrome |
| Nutritional status | Appears well nourished | Obese or thin. Generalized fat in simple obesity; truncal fat with relatively thin limbs in cushing's syndrome. |
| Behaviour/attitude | Appropriate reaction to the situation | Unusual behaviour, unexpected shaking movement, gestures, restlessness |
| Cleanliness/grooming | ood hygiene, clean clothing, well groomed | Dirty clothes, poorly groomed. |
| j)Speech [Listen for the pace of speech and its pitch, clarity, and spontaneity]. | Fast speech of hyperthyroidism, lack of spontaneity in depression, asthma. Slow, thick, hoarse voice of myxedema. |
- Skin:
- Use inspection and palpation. Start from the head then proceed down the body to the soles of the feet.
| Examination | Normal data | Abnormal data |
|
Inspect the skin for a) The colour. Note the colour change all over the body or in a localized area. Compare the right and left side. |
The colour varying from black, brown or fair depending upon the genetic factor. Uniform colour all over the body. No pallor, cyanosis, redness or yellowness |
Pallor due to anemia, peripheral cyanosis include anxiety, cold exposure and venous obstruction, central cyanosis include lungs disease, congenital Heart disease. |
| b) Any patches or lesions or any evidence of itching as shown by scratching. | Skin free of lesions or abrasion | Skin patches, lesions or itching present. |
| c) Edema | No edema | Edema |
| d) Excessive sweating or dehydration. | No excessive moisture or dryness. | Dryness in hypothyroidism, oiliness in acne. |
| e) Hair distribution, colour, cleanliness. | Clean, smooth and dry hair, colour of hair varying from black brown and white depending upon genetic factor, no colour change in the hair. | Loss of hair, dirty hair, changes in hair e.g. fine hair in hyperthyroidism, Coarse hair in hypothyroidism. |
| f) Evidence of injury | No bleeding, bruising or laceration of skin | Bleeding, bruising or laceration of skin |
|
Palpate the skin for: a) Temperature: Feel it with the back of fingers. |
Warm skin, even temperature | Generalized warmth in fever, hyperthyroidism, and coolness in hypothyroidism, local warmth in inflammation. |
| b) Texture: Feel the skin for smoothness. | Smooth, soft skin | Roughness in hypothyroidism |
| c) Edema: presses the skin with the index and middle finger and then leaves and watches the depression. | Quickly depression recovers | Depression recovers slowly |
| d) Dehydration: Dehydrated skin loses its elasticity. Check the elasticity of skin by pinching the skin just below the clavicle in adults and the abdominal skin in children, between the thumb and index finger, pulling it and quickly releasing it. | Elastic skin: The skin quickly comes back to its previous state. | Comes back to its previous state slowly |
- Lymph nodes:
- Use inspection and palpation
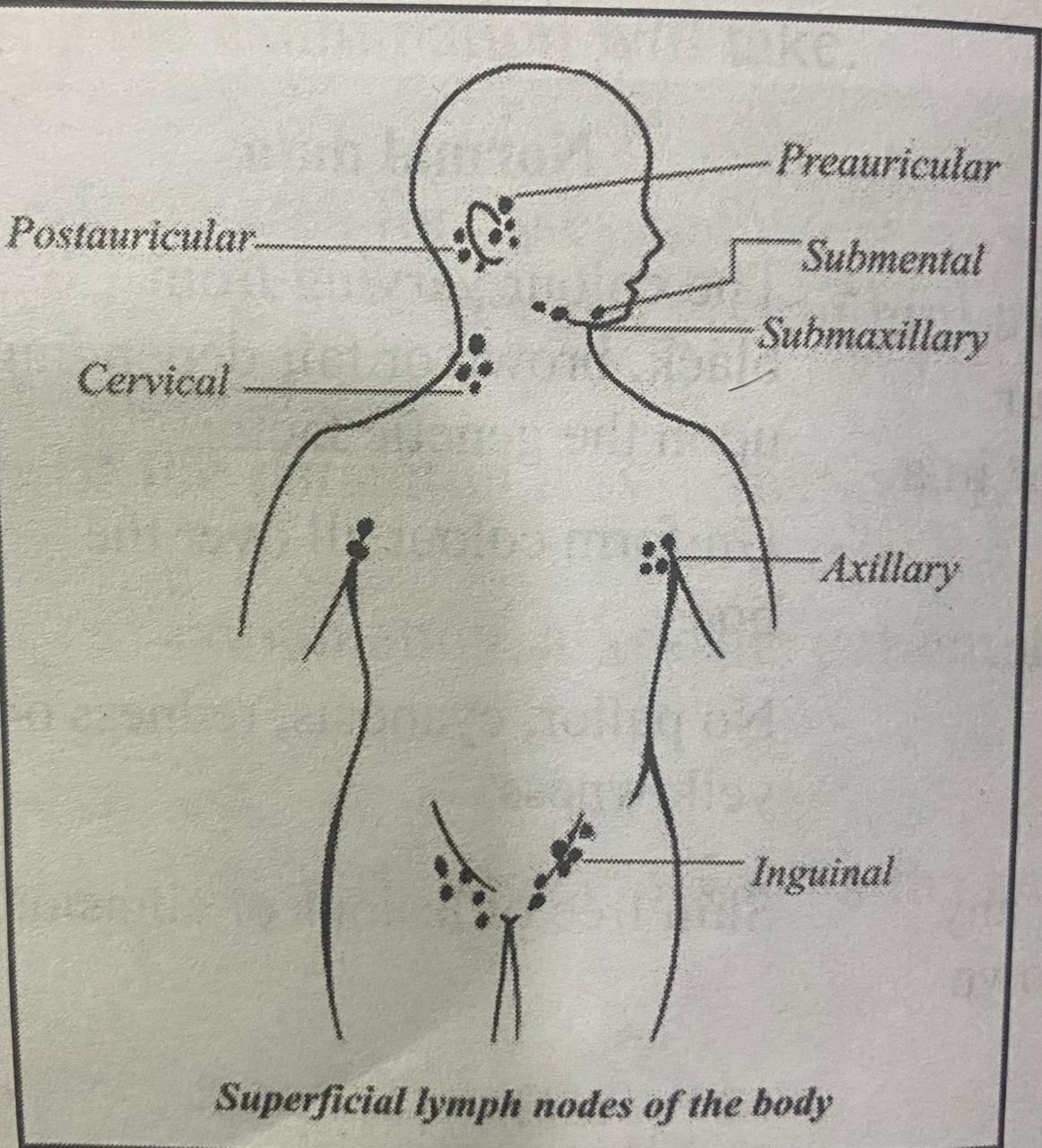
| Examination | Normal data | Abnormal data |
| Inspection Redness or enlargement of lymph nodes. | Lymph nodes not visible, no redness | Enlargement and redness of lymph nodes |
|
Palpation Enlargement and tenderness |
Lymph nodes are not palpable and tenderness | Hard, fixed nodes suggest malignancy, Enlargement of a supraclavicular node especially on the left, suggests possible metastasis from a thoracic or abdominal malignancy. |
- Head:
- Use inspection and palpation
| Examination | Normal data | Abnormal data |
|
Hair Inspect for: color, texture, growth and distribution. Palpate for: texture Scalp Inspect for: scaliness, lumps or other lesions |
Find coarse and looks strait to curly. No scaliness, lumps or other lesions. |
Excessive dry or oily, loss, pediculosis and dandruff Fine and silky hair in hyperthyrodysm Redness and scaling in seborrheic, dermatitis, psoriasis |
|
Skull: Inspection: General shape, size and contour of the skull. Palpation: Note any deformities, depression, lumps or tenderness. |
Head is symmetrical round and correct in the midline. | Enlarged skull in hydrocephalus |
|
Face Inspection: facial expressions, involuntary movements, edema and masses |
Relaxed facial expression, Uniform movement of sides of face, no edema and masses. |
Moon face in Cushing's syndrome, edematous face in Nephrotic syndrome, One side of the face moves differently from the other side indicating one sided facial paralysis. |
| Palpation: Swelling, tenderness and depression. |
No swelling, tenderness and depression. |
Swelling, tenderness, and depression. |
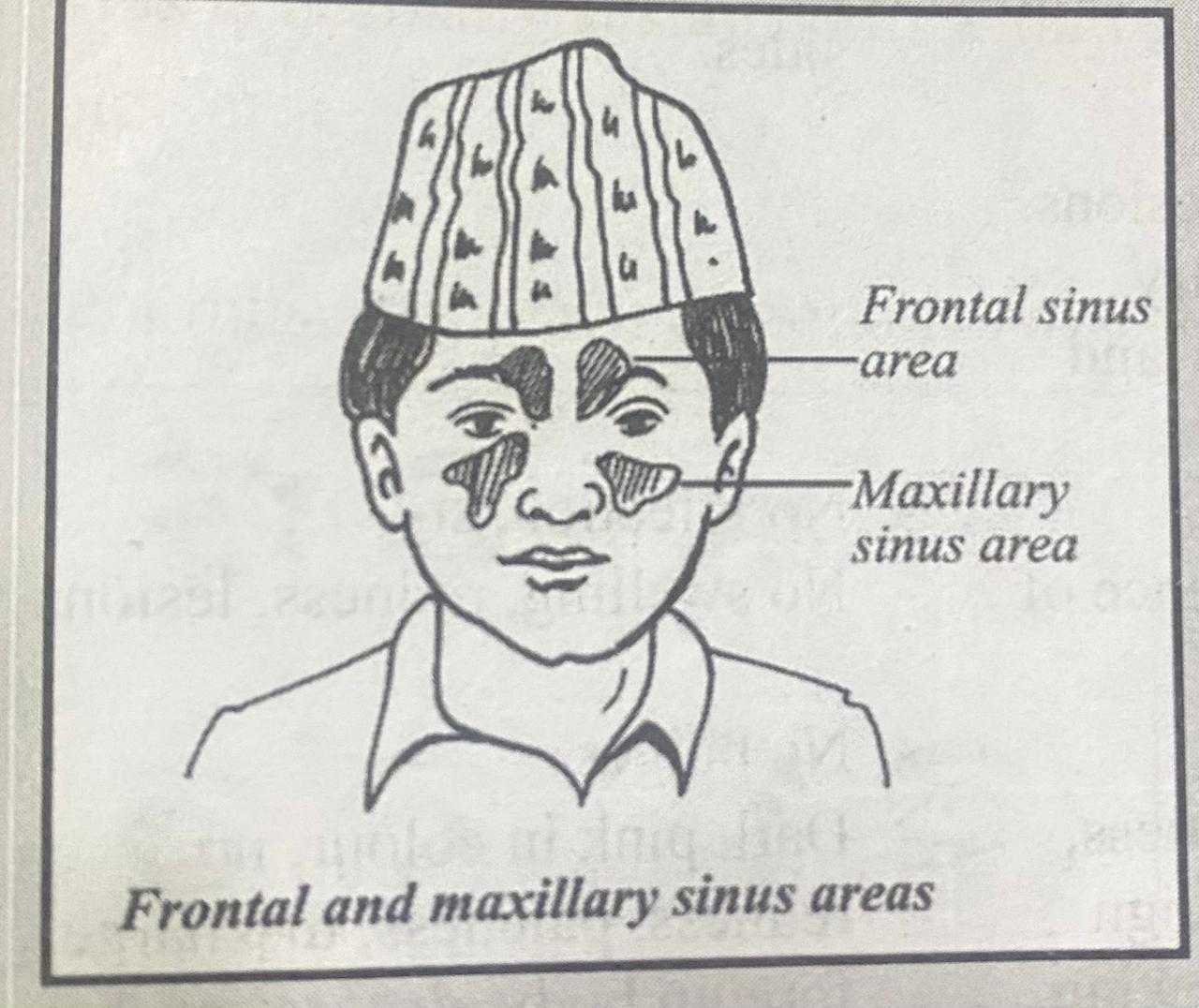
- Sinuses:
- Use inspection and palpation
| Examination | normal data | abnormal data |
| Palpate the sinuses Palpate for frontal sinuses tenderness by pressing up from under the bony brow on each side. Avoid pressure on the eyes. Then press up on each maxillary sinus. |
No tenderness in frontal and maxillary sinuses
|
Local tenderness, together with symptoms such as pain, fever, and nasal discharge, suggest acute sinusitis involving the frontal or maxillary sinuses. |
|
the Transillumination of the sinuses -Transillumination is not routine, it is often helpful when sinus tenderness or other symptoms suggest sinusitis. The room should be thoroughly darkened. Using a strong, narrow light place the light source, place snugly deep under each brow, close to the nose. Shield the light with your hand. Look for a dim red glow as light is transmitted through the air-filled frontal sinus to the forehead. |
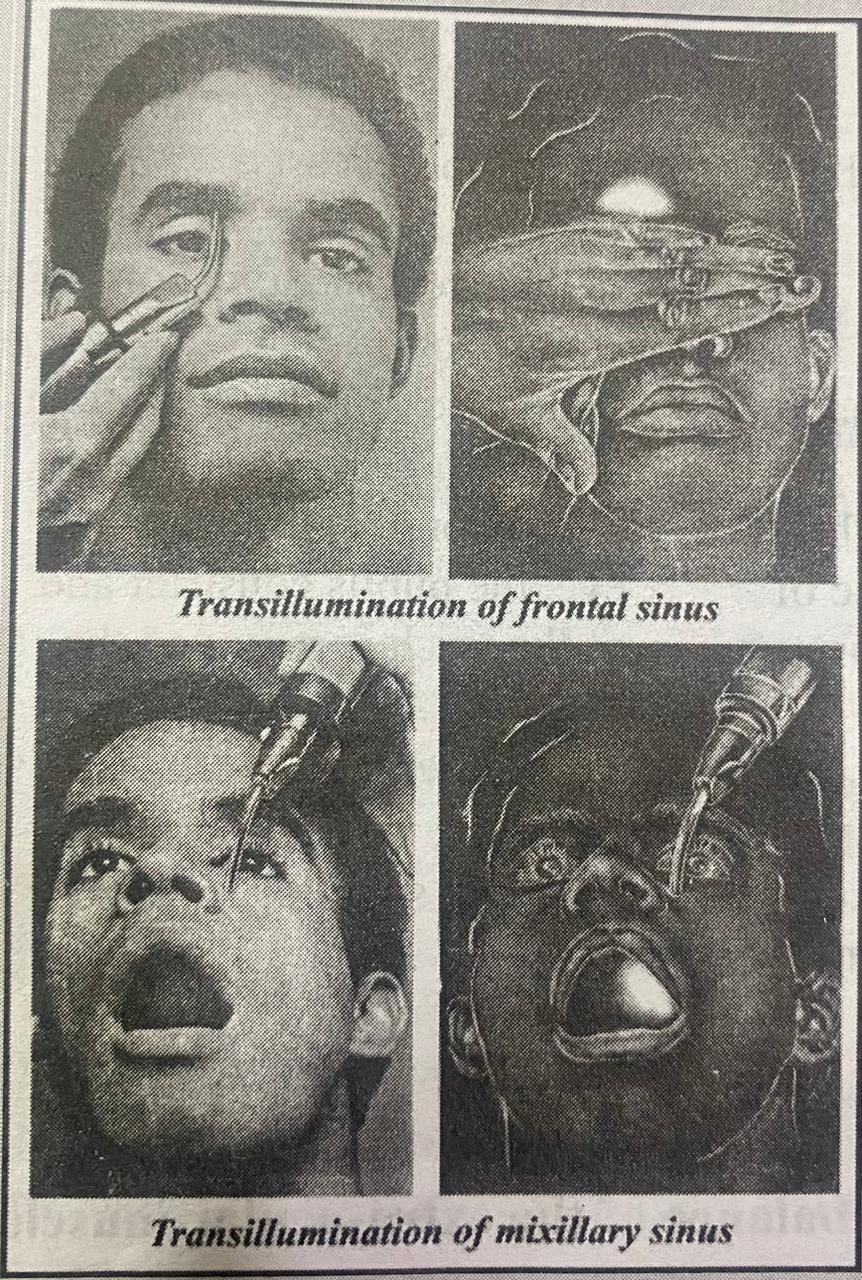 |
Absence of glow on one or both sides suggests a thickened mucosa or secretions in the frontal sinus, but it may also result from developmental absence of one or both sinuses. |
| Ask the patient to open the mouth wide and tilt the head back. [An upper denture should first be removed.] Shine the light downward from just below the inner aspect of each eye. Look through the open mouth at the hard palate. A reddish glow indicates a normal air- filled maxillary sinus. |
- Eye:
- Use inspection and palpation
| Examination | Normal data | Abnormal data |
|
Inspection Stand in front of the client and inspect the both eyes for position and alignment. Observe for Ptosis, exophthalmos, lesions, deformities or asymmetry. Eye brows: distribution and quantity |
No deviation and abnormal profusion Equal distribution in both sides. | Inward and outward deviation Abnormal profusion in disease or ocular tumours Ptosis, entropian, extropain - Exophthalmoses is caused by hypothyroidism Absent or abnormally distribution |
| Eye lashes |
No infection, sty |
Present infection, sty |
|
Eye lids: position, presence of edema, lesions. |
No swelling, redness, lesions | Present swelling, redness or lesions |
| the eye for bulges | No bulges | Bulging, staring or sunken eye. |
|
Conjunctiva for any redness, paleness, discharge, foreign body, dryness or tear flowing. |
Dark pink in colour, no redness, paleness, discharge, foreign body, dryness or tear flowing; it is just moist. | Pale palpebral conjunctivas indicate anemia, and Redness indicates conjunctivitis. |
| The sclera for any colour change, injury and dilated blood vessels. | White in colour with few small blood vessels |
Yellow sclera indicates jaundice |
| The cornea for colour, abrasions or white spots. |
Transparent, no abrasions or white spots |
Cloudy appearance, abrasions or white spots |
|
The pupils for size and shape;compare both the pupils. |
Pupils are round and uniform in size and shape | Irregular size or shape of the pupil |
|
The pupil's reaction to light. Light a torch from the side of the eye and remove it. Observe how the pupil reacts. |
As the torch approaches the eye, the pupils constrict and as the torch is removed the pupils dilate | Pupils remain constricted even after the torch is removed |
| The lenses for opacities (Lens is situated just behind the pupil.) | transparent | White, cloudy lens |
| Lacrimal apparatus: inspect the region of the lacrimal gland and lacrimal sac for swelling Look for excessive tearing or dryness | No lump swelling, normal tearing | Lump, swelling, excessive tearing due to infection, increased production. Dryness |
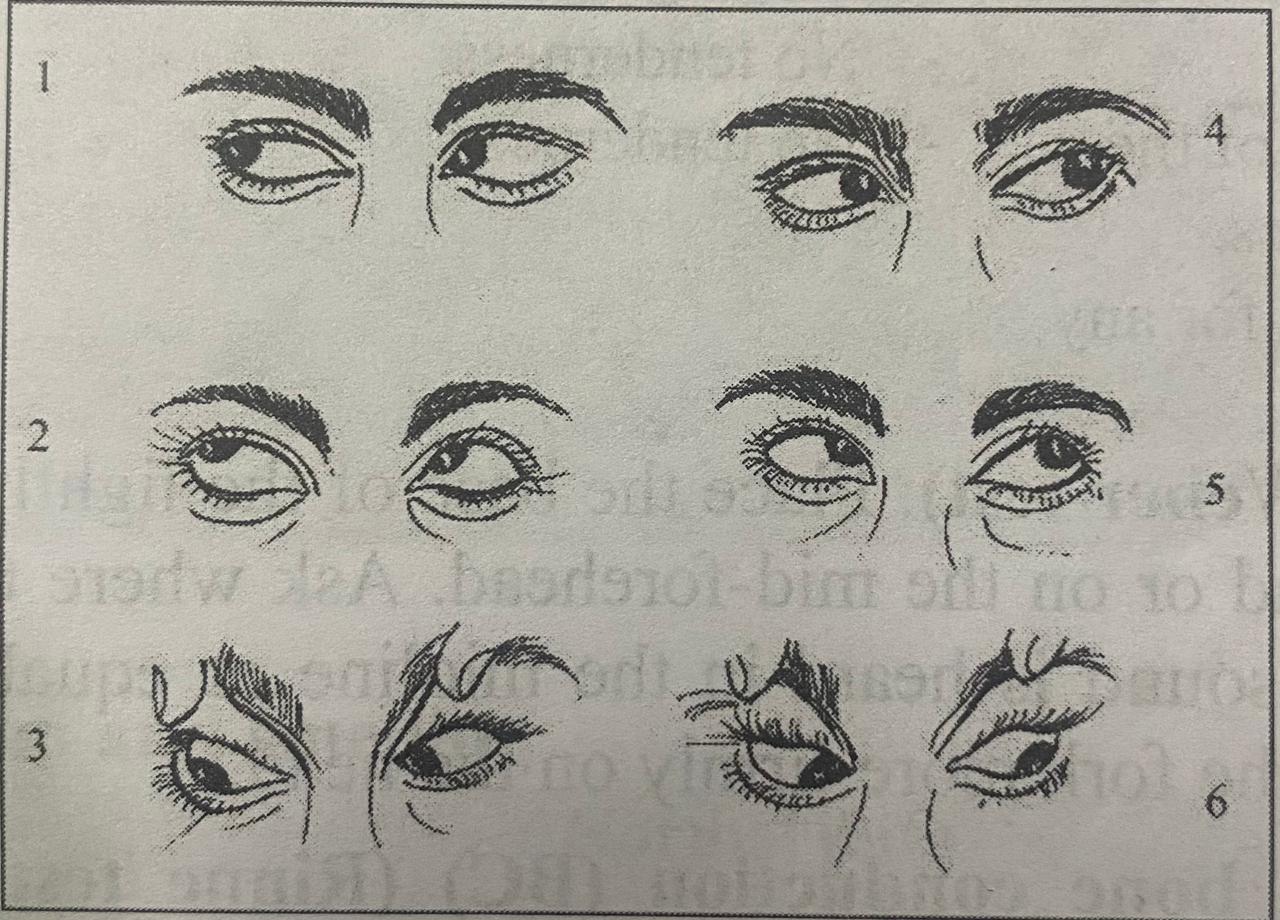
Look for weakness or imbalance of the extra-ocular muscles
To assess the extra-ocular movements, stand or sit 3 to 6 feet in front of the patient. Ask the patient to follow your finger or pencil as you sweep through six cardinal directions of gaze. Making a wide H in the air leads the patient's gaze.
- Extreme right.
- To the right and upward.
- Down a right.
- To the extreme left.
- To the left and upward.
- Down on the left.
Asymmetry of the corneal reflection indicates a deviation from normal ocular alignment which may be caused by muscle weakness.
Inspect for normal conjugate or parallel, movements of the eyes in each direction, or any deviation from normal.
Convergence test
Ask the patient to follow your finger or pencil as you move it in toward the bridge of the nose. Note convergence of the eyes. This is normally sustained to within 5 cm to 8 cm. Poor convergence in hyperthyroidism
Cover test
A cover test may bring out a latent muscle imbalance not otherwise seen.
Testing vision
Visual acuity is a test of central vision. If possible use a snellen eye chart and light it well. Position the patient 20 feet from the chart. Patients who use glasses other than reading glasses should wear them. Ask the patient to cover one eye with a card and to read the smallest line of print possible. Record the smallest line the patient read successfully. Normal finding is 6/6. Unexpected loss of acuity is a sign of serious ocular pathology.
Visual fields by confrontation
It is rough clinical test of peripheral vision. This procedure is usually omitted in a routine examination but should be included whenever a neurological problem is suspected.
Method
Ask the patient to cover one eye without pressing on it, and to look at your eye directly opposite. Close your other eye. Slowly bring a pencil or other small test object from the periphery into the field of vision from the 8 direction and ask the patient to say 'now' as soon as it appears. During most of this examination keep the test object equidistant between your eye and the patient's so that you can compare the patient's visual field your own. Repeat with the other eye.
- Ear:
- Use inspection and palpation
| Examination | Normal data | Abnormal data |
|
Inspection -location |
The top of the pinna meets or crosses the eye imaginary line drawn from the occiput line outer canthus of the eye to the occipital protuberance. | The top of the pinna does not meet or cross the eye-occiput line. |
| The pinna for any lump or lesions | No lump or lesion, smooth rounded contour | Lump or lesion |
|
External auditory canals for any ear discharge, redness, mass, foreign body or cerumen (a waxy substance produced by ceruminous gland in the outer portionof the canal ) _ pull the upper portion of pinna upward and backward to straighten the canal in the adult patient - use torch or otoscope to visualize ear canal |
No discharge, redness, mass or foreign body, slight cerumen present | Clear blood or yellow discharge, redness, mass, foreign body, excessive cerumen present |
| tympanic membrane | -no performance lesions, bulging | perforations, lesions,bulging |
|
Palpate the ears by -pulling the upper portion of the pinna a little for tenderness -pressing the mastoid area for any tenderness |
-no tenderness -NO tenderness |
-Tenderness -Tenderness behind the ear may be present in otitis media |
Test for lateralization (Weber test): Place the base of the lightly vibrating tuning fork firmly on top of the patient's head or on the mid-forehead. Ask where the patient hears it: on one or both sides. Normally the sound is heard in the midline or equally in both ears. If nothing is heard, try again, pressing the fork more firmly on the head.
Compare air (AC) and bone conduction (BC) (Rinne test): Place the base of lightly vibrating tuning forks on the mastoid bone, behind the ear and level with the canal. When the patient can no longer hear the sound, quickly place the forks close to the ear canal and ascertain whether the sound can be heard again. Here "U" of the forks should face forward, thus maximizing its sound for the patient. Normally the sound is heard longer through air than through bone (AC>BC).
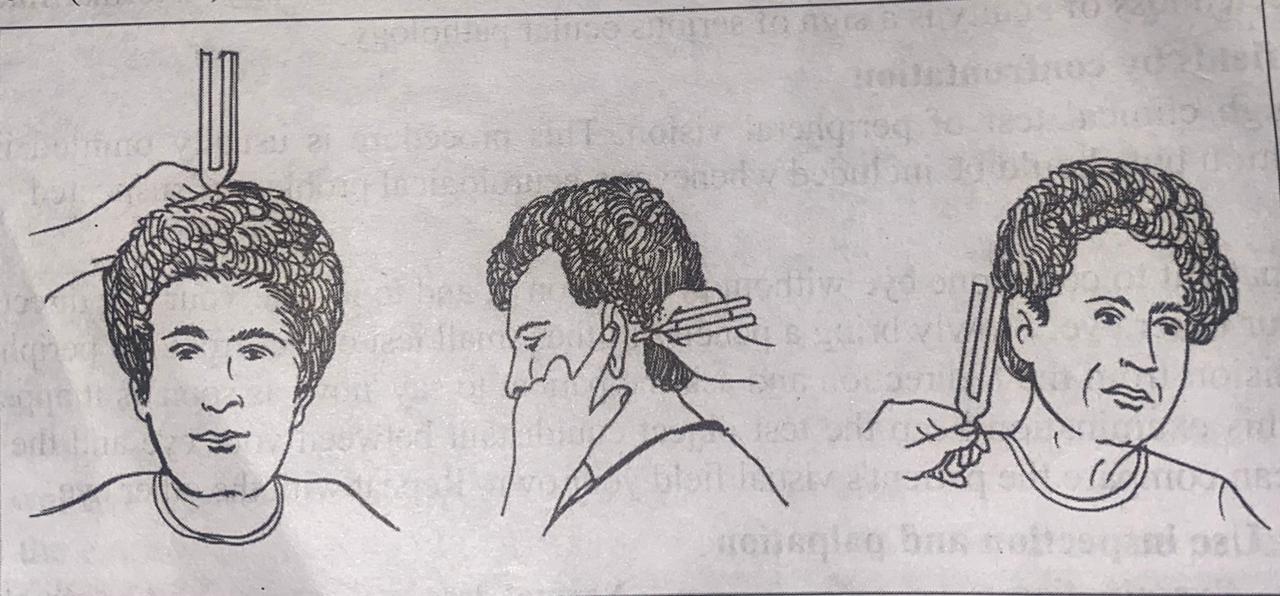
Weber test Rinne
Voice test: whispered is a high frequency sound and is used to detect high tone loss. Test one ear at a time.
- Nose:
- Use inspection and palpation
| Examination | Normal data | Abnormal data |
|
Inspection -Location of nose |
-centrally located | -Deviated in location |
| -The nostrils for their size, and flaring | -Nostrils are uniform in size and do not flare | -Asymmetrical in size or flaring nostrils |
| The nasal septum for any polyps (growths) | No polyp or deviation | Presence of polyps or deviation. |
| The nasal canals with a torch for redness, discharge, foreign bodies, etc. | Dark pink mucous membrane, no discharge or foreign bodies. | Red swollen mucosa of acute rhinitis; pale mucosa of allergic rhinitis. |
| Palpate external nose for: tenderness, masses and displacement of bole and cartilage. | ||
|
Check the nasal passage is clear or not Test the sense of smell for each nostril separately. Ask him her to identify the source of smell using familiar non-noxious smell. |
have no sense of smell | Cannot smell in respiratory infection and sinusitis. |
- Mouth and Throat
- Use inspection and palpation and smelling
| Examination | Normal data | Abnormal data |
|
Inspect -The lips for colour, moisture, lumps, cracks or ulcers. |
- Pink, moist and intact skin, no bluish discoloration, cracks and ulcers. | - Lips bluish in colour cracks or ulcers present. |
| - The mucous membrane of the mouth for the colour, ulcer, nodules and amount of saliva. | - Pink, moist mucous membrane .no ulcer, nodules. | -Blue, red or pale mucous membrane. Excessive or less amount of saliva. |
| -The gums for inflammation, swelling, redness or bleeding. | - Pink, no inflammation,
swelling, redness or bleeding |
-Inflammation, swelling, redness or bleeding present. |
| - The teeth for the colour, caries (teeth with black spots indicating cavities) and missing teeth. | -White teeth, no caries and missing teeth | -Brown teeth, presence of caries or missing teeth. |
| -The tongue for symmetry, colour and papillae. | -Symmetrical, pink, moist, papillae and midline fissure present | - Asymmetrical, red, pale, dry papillae or fissure absent. |
| -The throat and note the colour and size of tonsils. | -Pink throat and small tonsils | -Red swollen and yellow discharge on the tonsils. |
| -The swallowing difficulty by asking the patient to swallow. | -No difficulty in swallowing | difficulty in swallowing |
|
Palpate -The gums on both sides with fore fingers of the right hand and check for swelling and tenderness (use gloves if available) |
- No swelling, no tenderness | -Swelling and tenderness present |
| -The teeth by moving them with the fore fingers of the right hand for any pain or loose teeth. | -No toothache, no loose tooth | -Toothache or loose teeth present. |
|
Smell -The patient's breath and note any foul odour, or alcohol smell in the breath. |
-No foul odour nor smell of alcohol | -Breath odour of alochol, acetone in diabetes mellitus,pulmonary,infection, uremia etc. |
- Neck use inspection and palpation
| Examination | Normal data | Abnormal data |
|
-The neck by asking the patient to sit straight. Note the position of the head and neck. -Ask the client to sip some water, to extend the neck, and swallow. Observe for upward movement of the thyroid gland, -Observe masses, and scars of neck. |
-No tilting of head No masses, scars |
-Tilting of head -A scar of past thyroid surgery may be the clue to unsuspected hypothyroidism. |
| -Enlargement of thyroid gland. | - Thyroid gland not visible and enlarged | -Enlarged thyroid gland. |
| -For the ability to move neck up and down and from side to side. Note any stiffness or tenderness.
-The back of neck for any swelling or lump |
- Full and smooth range of movement, no stiffness or tenderness. - No swelling or lump |
-Swelling, tenderness and decreased range of motion suggest arthritis. -Swelling or lump present |
|
Palpation -Entire neck for enlarge lymph nodes -The back of neck along the spine and back of the head. Check for the muscle tightening, tenderness, lump, etc. Palpate the thyroid gland -Move behind the client -Ask the client to flex the neck slightly forward to refax the sternomastoid muscles. -Place the fingers of both hands on the client's neck so than your index fingers are just below the cranial cartilage. -Ask the client to sip as swallow water as before. Feel for the thyoride isthmus rising up tender your fingers pads. -Displace the trachea to the right with the right hand fingers, palpate laterally for the right lobe of the thyroid in the space between the displaced trachea and the relaxed sternomastoid. Find the lateral margin. Examine the left lobe in same way. |
- Normally trachea is in midline -No tightness of neck muscles. No tenderness along the spine. -Normally you cannot palpate the thyroid gland. |
-Goiter as a general term for an enlarged thyroid gland -Muscle tightening, tenderness along the spine, lump along the spine. -Diffuse enlargement in endemic goiter -Soft in Graves disease -Firm in malignancy -Tenderness in thyroiditis -Multinodular goiter is additional factors for malignancy
|
- Chest and Lungs:
- Use inspection, palpation,percussion and ausculation
| Examination | Normal data | Abnormal data |
|
Inspect the chest for -size and shape. not the anteroposterior and lateral diameters of the chest. |
-Lateral diameter (side to side) is winder than the anteroposterior (front to back) diameter |
-Barrel shaped chest (increase antero-posterior diameter) due to pulmonary emphysema -Funnel shaped chest: Characterised by a depression in the lower portion of the sternum. -Pigeon shaped chest: sterum is displaced anteriorly and increasing anterioposterior diameter. |
| -The symmetry. Note the location of sternum. | -Symmetrical shape, sternum is located at the midline. | -Sternum is displaced |
| -The expansion during breathing. | -Even expansion of the chest | -Uneven expansion of the chest. |
| -The intercostal spaces whether they move in (retract) when the patient breathes in. | -No intercostal retraction | -Retraction at the intercostal spaces. |
| -The cough. If the patient has a cough, ask him to cough up the sputum and check the amount and colour sputum. | -No cough, no sputum | -Brownish grey, yellow, green, bloody or frothy sputum. |
|
Palpation -Anterior and posterior thorax: Check for tenderness, lumps, depression along the ribs. -Respiratory excursion, tectile fremitus. -The chest for expansion. Place both hands flat against the chest with the thumbs in midline. The hands will move with chest expansion during deep breathing. Watch for the even expansion of the chest on both sides. |
-No tenderness, lump or depression along the ribs
-Even expansion of the chest on both sides. |
- Tenderness of the chest lump or depression along the ribs present -Uneven expansion of the chest or limited expansion. |
|
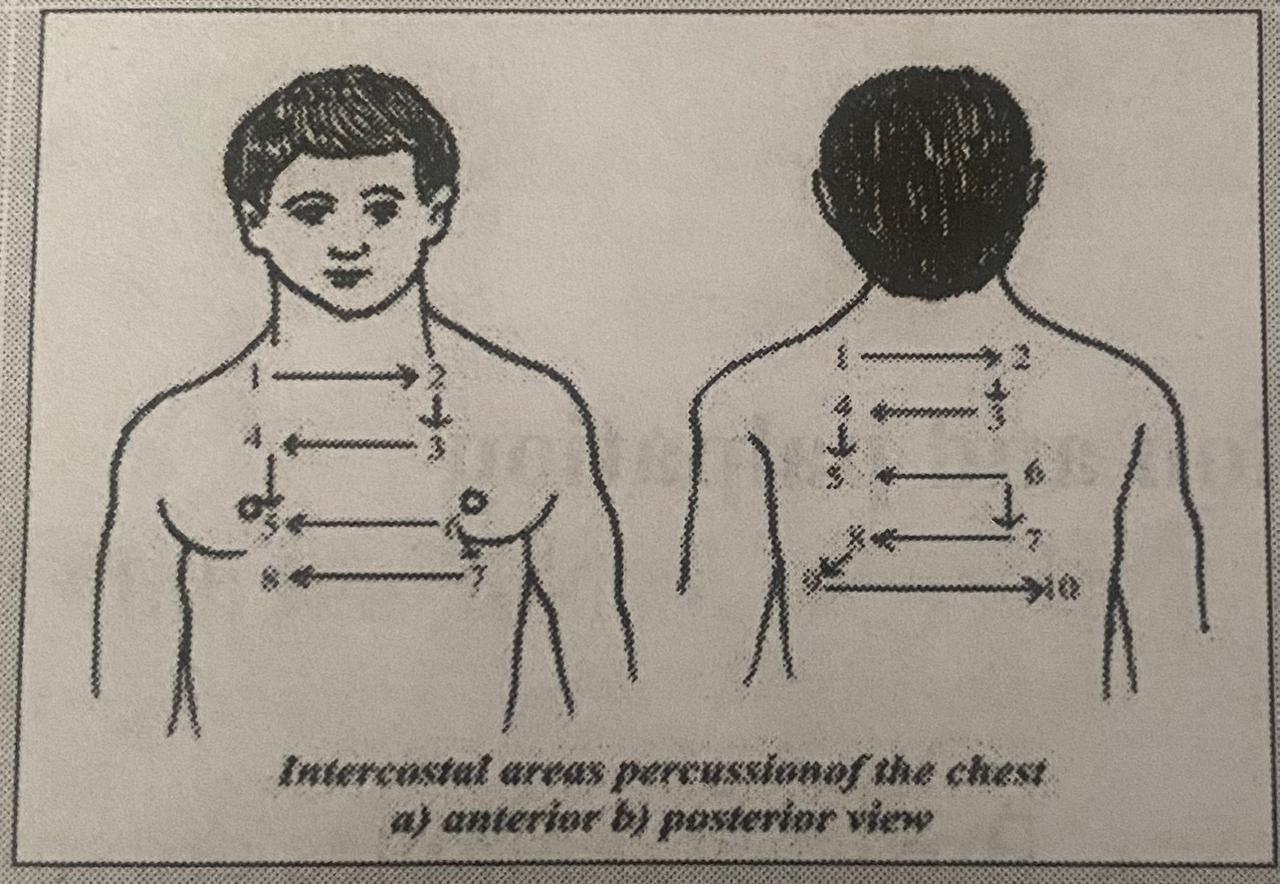
Percussion -The front and then the back of the chest. Place the patient in the sitting position to percuss the posterior chest from the apex to the base to find out whether the lungs are filled with air or fluid. |
-Deep resonant sound over the lungs. |
-Dull, flat or hyper resonant sound over the lungs. |
|
Auscultation -The front as well as the back of the chest to evaluate the breath sound by using stethoscope, ask the patient to take deep breathing and auscultate the chest. -To compare the duration of inspiration and expiration. -Check for any abnormal sounds like rales, (fine crackling sounds). Rhonchi (loud bubbly sounds) and wheezing. |
-Breath sounds are heard in all areas of the lungs - Inspiration longer than expiration- No rales, rhonchi and wheezing sounds. |
-Absent or decreased breath sounds. -Prolonged expiration. -rales, rhonchi, wheezing Sounds, pleural rub, crepitations present. |
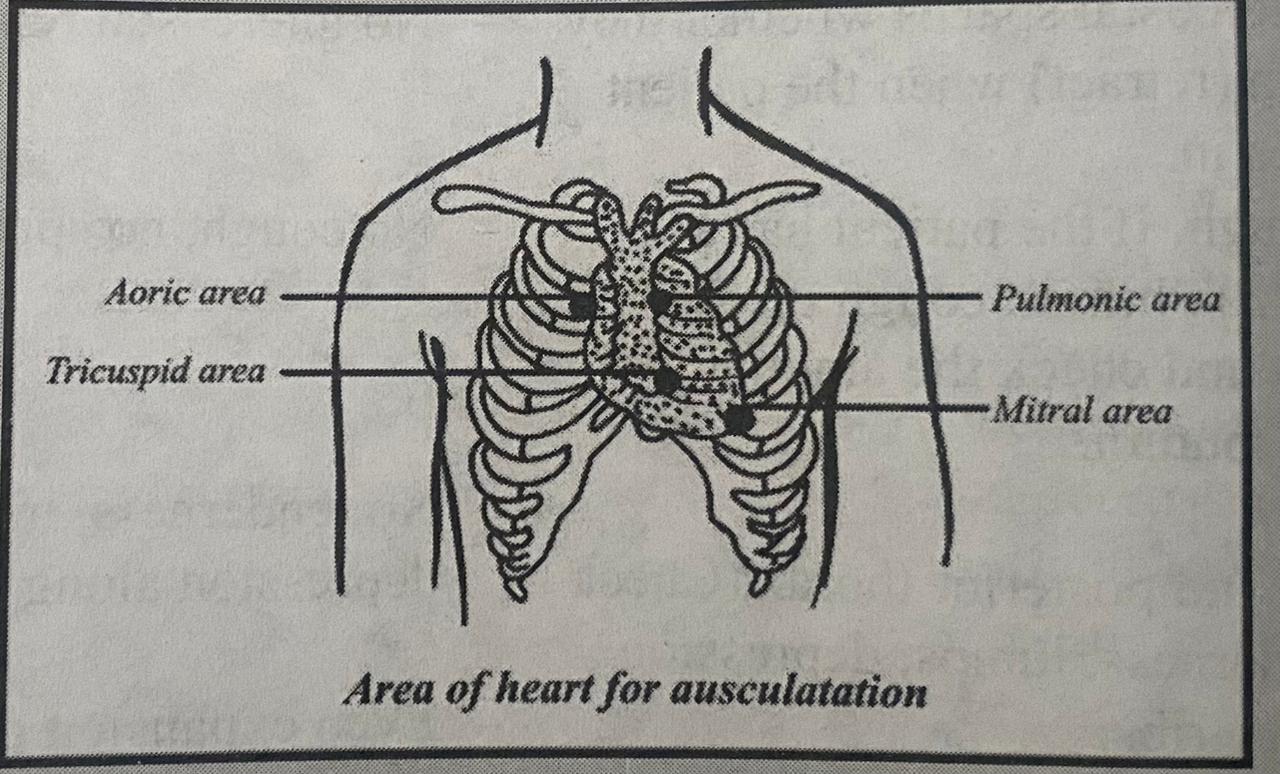
- Heart:
- Use inspection and auscultation
| Examination | Normal Data | Abnormal Data |
|
Inspection -Enlargement of neck vein. Auscultation -Aortic area (second intercostal space just to the right of the sternum). -Pulmonic area (second intercostal space just to the Left of the sternum). -Tricuspid area (fourth intercostal space just to the left of the sternum). |
-No enlargement
|
-Enlargement- |
|
-Mitral area (fifth intercostal space at the midclavicular line). -Note the clarity and regularity of the heart sounds. Count the heart beat rate at the areas and compare with the radical pulse to detect skipped beat by using stethoscope. |
-Clear and regular, heart rate, 60-80 beats per minute. No murmur sound present. |
-Decreased or inaudible heart sounds irregular or missed heart beats. Heart rate less than 60 or more than 80 beats per minute. Murmur sound present. |
Male Breast: A firm dise of glandular enlargement in a male in called gynecomastia
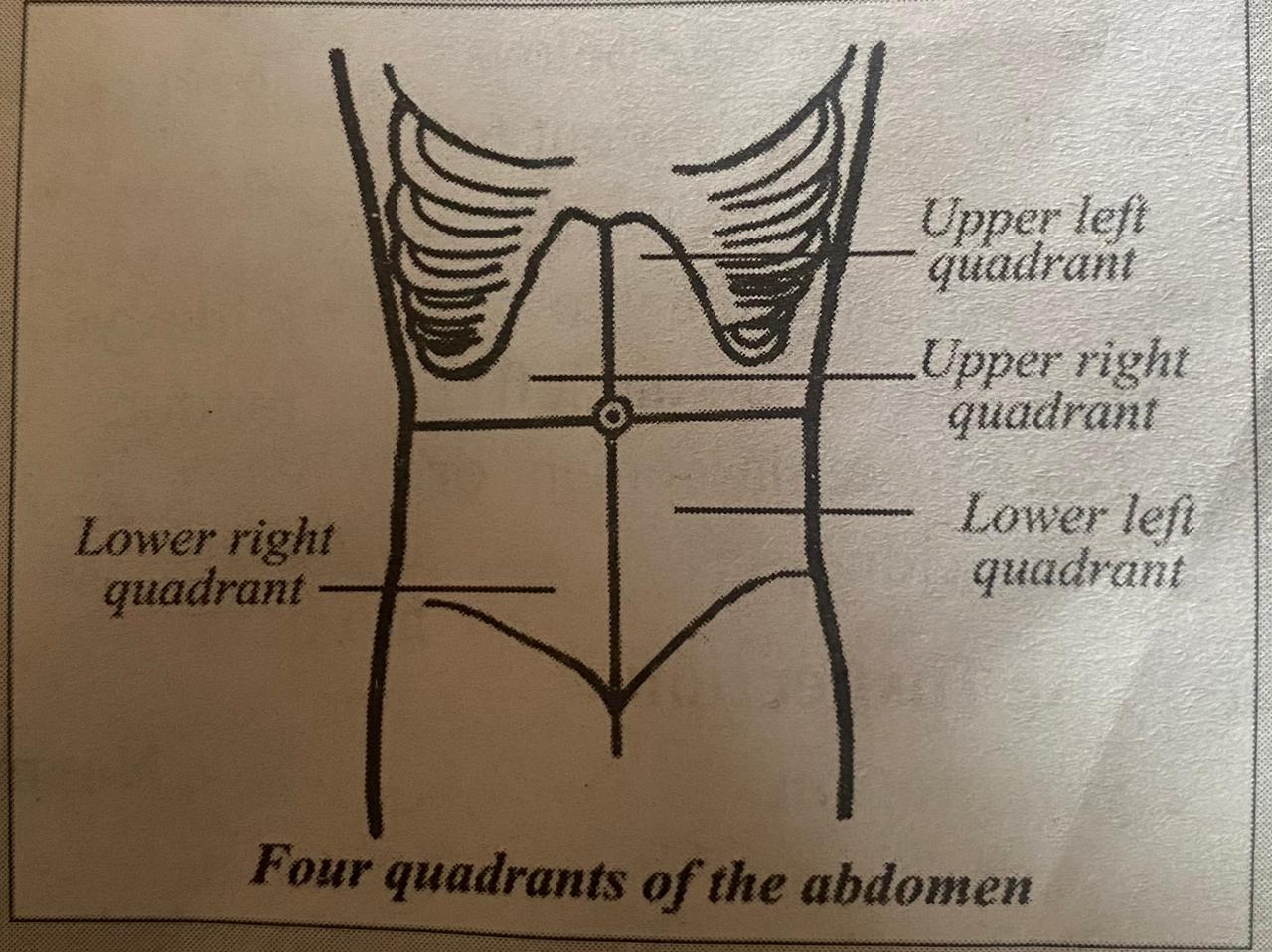
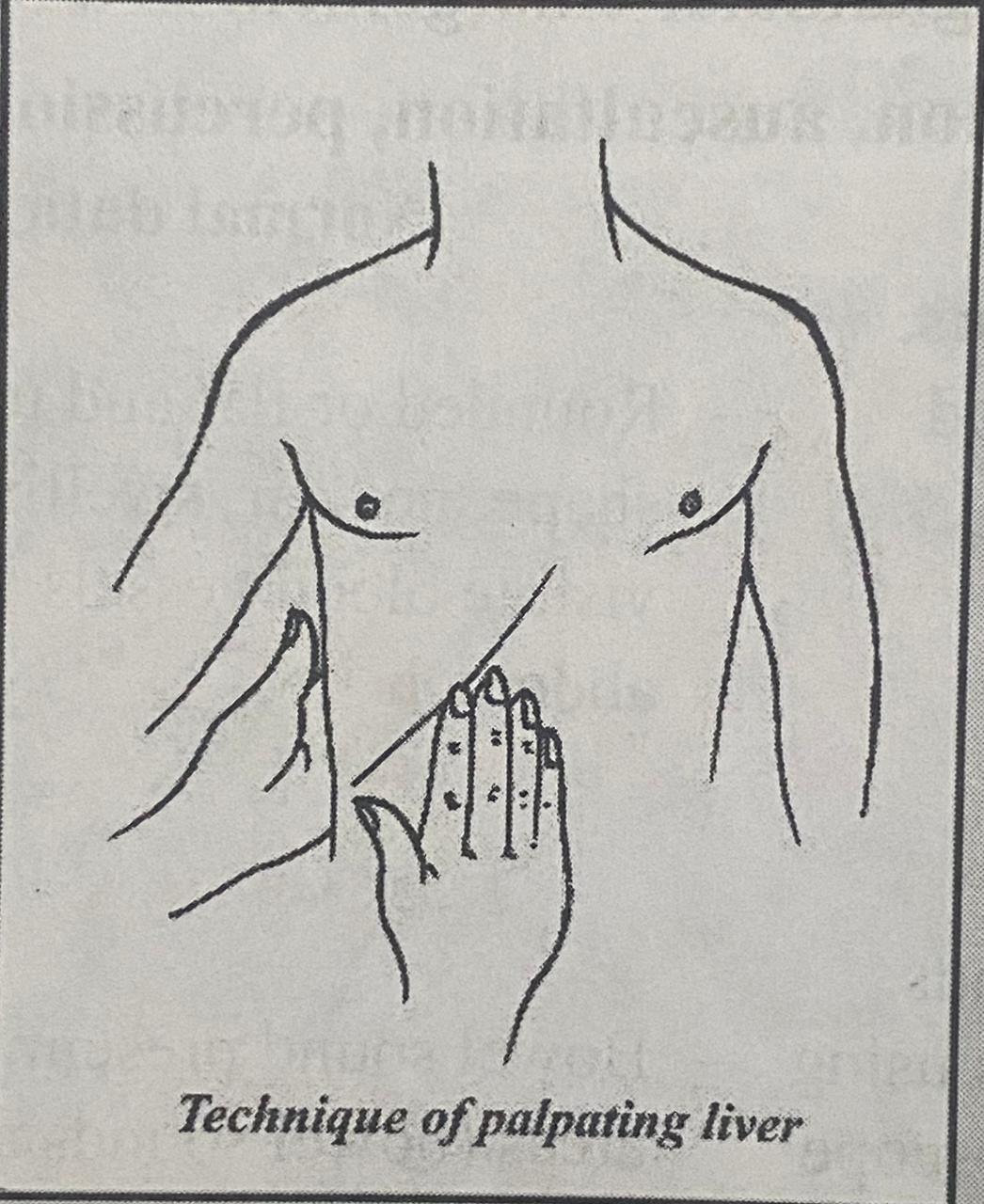
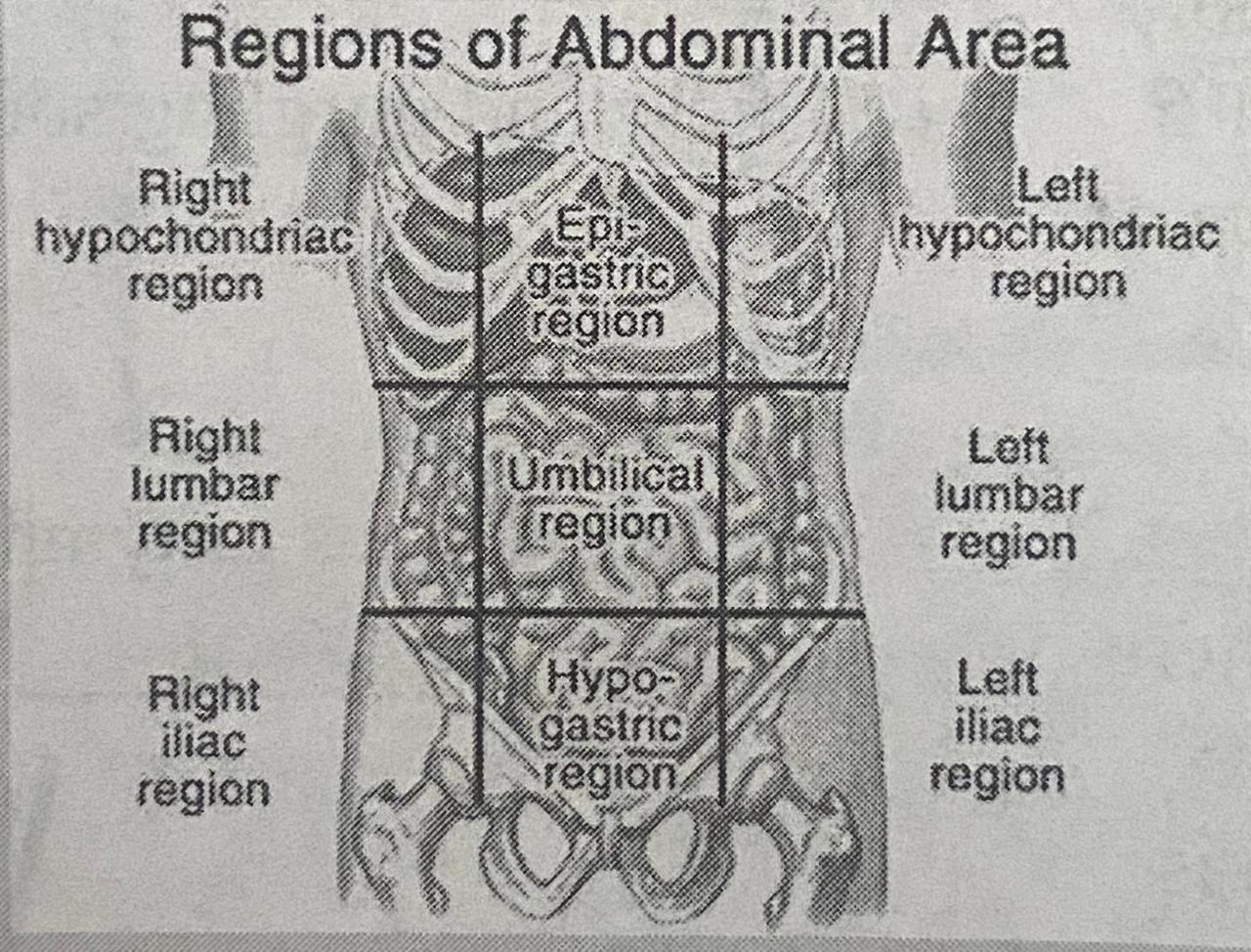
- Abdomen:
- Use inspection, ausculation, percussion and palpation
| Examination | Normal Data | Abnormal Data |
| Inspection: For the shape, scars, swelling and distended blood vessels. | -Rounded or flat and uniform shape, no scar, swelling and visible blood vessels in abdomen | -Irregular in shape, abdominal scars present indicating previous injury or surgery. Swelling of abdomen and distended blood vessels. |
| Auscultation: For bowel sounds. Listen carefully in all areas using the stethoscope. The stethoscope should be warm as the cold may contract the abdominal muscles. Note whether the bowel sounds are increased; decreased or absent. If bowel sound is not heard, listen in all areas for 5 minutes. (Note also the type of sound.) |
-Bowel sound present in all areas (bowel sounds are produced in every 5-15 seconds). -Clicks and gurgling sounds. |
-High pitched tinkling sounds, absence of bowel sound (no bowel sound heard for 5 minutes).
-Loud rushing sound. |
|
Percussion -Keep the patient in supine position. Note the areas where dull or tympanic sounds are produced (tympanic sound is heard over gas-filled viscera and dull sound over fluid-filled viscera, faecal organs or masses). Then turn the patient on his side. Again percuss all the areas. Note if there is shifting dullness when the patient is moved. Shifting dullness is a sign of fluid in the abdomen. |
-Scattered areas of tympany and dullness
|
-Absence of tympany |
|
Palpation -Place the patient in the supine position and ask him to relax his abdomen. Palpate the abdomen in all four quadrants. Feel for any masses or tenderness. -The liver: Place the left hand on the back beneath the patient's 11th and 12th rib and apply upward pressure to push the liver forward towards the examining right hand. Place the palmar surface of the right hand parallel -to the costal margin. Ask the patient to take a deep breath and as the patient inspires feel for the liver sliding over the fingers. Not any enlargement or tenderness. If enlarged, estimate the amount of enlargement beyond the right costal margin. Express it in centimeters. - The spleen: Keep the patient in right lateral position. Place the left hand on the patient's back under the left rib cage. Apply upward pressure in the left upper quadrant with the right hand fingers moving towards the anterior axillary line and beneath the costal margin. Feel for the enlargement or tenderness of the spleen. -Kidneys: Keep the patient in the supine position. Place the left hand on the patient's back between the lowest rib and the pelvic bone. Place the right hand on the patient's right side below the lowest rib. Ask the patient to take deep breaths. Press firmly with the right hand and try to feel the kidney. Feel on the left side too. Note the enlargement or tenderness on kidneys.
|
-No abdominal mass and tenderness.
-Liver is not usually palpable but in thin people may be palpable immediately below the costal margin as a smooth structure with a regular contour and a firm, sharp edge.
-Spleen is not palpable; no enlargement and tenderness on palpation
-Kidneys are not palpable and tender. |
- Abdominal mass and or tenderness.
-Liver palpable as soft or hard edge or irregular in contour.
-Spleen, enlarged and tender - Kidneys enlarged and tender. |
- Anus:
- Use inspection
| Examination | Normal data | abnormal data |
|
Inspection -The anus for any irritation, crack, fissures or enlarged vessels. |
-No irritation, fissure, cracks, or enlarged blood vessels in the anus. | -Presence of anal irritation, anal fissure and enlarged anal blood vessels. |
- Male genitals:
- Use inspection, palpation
| Examination | Normal data | Abnormal data |
|
Inspection -The penis for any sores or lumps. -The scrotum for any redness, swelling or any lesions. |
-No sore, lump. - No swelling, redness or lesions |
-Presence of sore or lump. - Swelling, redness or lesions of scrotum.
|
|
Palpation -Enlargement or tenderness of scrotum palpate testes. |
-No enlargement, tenderness of scrotum. Testes are equal in size, no tenderness. | -Enlargement or tenderness of scrotum, one testis is largel than the other. |
- Female genitals:
- Use inspection
| Examination | Normal data | Abnormal data |
|
Inspection -The labia for colour and look for redness or swelling of the labia. -Check the urethral orifice for redness or discharge. -Look for any discharge or bleeding from the vagina. |
-Labia are of the same colour and size; no redness or swelling of the labia. -No redness or discharge at the urethra. -No unusual discharge from the vagina, no bleeding from the vagina (except during menstruation). |
-Red or swollen labia.
-Redness or discharge at urethra. -Unusual discharge and bleeding (Except during menstruation). |
- Muscular-Skeletal System:
- Use inspection and palpation
| Examination | Normal data | Abnormal data |
|
Inspection -The muscles and joints. Ask the patient to stand. Inspect his neck, shoulder, arms, hands, hips, knees, legs, ankle and feet. Compare one side with the other side. Note any bone or joint deformity, joint redness, swelling or muscle wasting. -The joint movement. Ask the patient to move his neck, shoulders, elbows, wrists, etc. |
-No bone or joint deformity, no redness, swelling of joints, no muscle wasting. -Able to move joints freely no sign of pain while moving joints. |
-Presence of bone deformity, joint deformity, joint redness or swelling, muscle wasting. Limited movement of the joint; signs of pain when moving the joint. |
|
-Fingers, hip, knees, ankles, and toes one by one in all possible directions. -Make a fist with each hand, thumb across the knuckles, and then extend and spread the fingers. -The patient's spine. Note its placement and curvature. |
-A person able to make tight fists and extend and spread the fingers smoothly and no easily. ora -Spine is in the s midline; spine slightly curved out form the neck and gradually curving inward at the waist. |
-Conditions that impair range of motion include arthritis, inflammation of the tendon sheaths and fibrosis in palmer fascia. -Lateral deviation of spine, increased curvature of spine, increased curvature of spine or flattening of curves of the spine. Decreased spinal mobility in osteoarthritis. |
|
Palpation -The musculo-skeletal system e.g. the patient's neck, shoulder, elbows, wrist, fingers, hips, knees, ankles, toes one by one and feel for swelling, tenderness and temperature. -Range of motion at knees and hips. Ask the patient to bend each knee in turn up to the chest and pull it firmly against the abdomen. Observe the degree of flexion at the hip and knee. In addition, note whether the opposite thigh remains on the table and thus can fully extend. |
-No joint swelling or tenderness - Normal temperature |
- Joints swelling suggests rheumatoid arthritis if it is bilateral and lasts for several weeks. -Increased temperature over a joint. -Flexion of the opposite thigh indicates a flexion deformity of that hip |
- Nervous System:
- Use inspection and palpation
| Examniation | Normal data | Abnormal data |
| -Muscle strength: Push against the patient's hands and feet and ask him to resist the push. | -Equal strength in both hands and feet; no muscular weakness. | Muscular weakness in one or both hands and feet. |
| -Sensation: Ask the patient to close his eyes. Brush the skin of his face, arms, hands, thighs and legs with a piece of cotton and instruct the patient to signal when he feels light brush of the cotton. | -feels light brush of the cotton equally on both sides of his body. | Loss of sensation to light brush. |
| -Co-ordination of movement: Ask the patient to button his shirt or to tie his shoes. | -Co-ordinated movements | Uncoordinated movement. |
| -Assess deep tendon reflexes | Presence of all reflexes |
Absent/ hyperactive/ hypoactive |
- Reflexes
- Biceps reflex (C5-C6)
- Partially flex the patient's arm at the elbow, and rest the forearm over the thighs placing the palm of the hand down.
- Place the thumb of your non- dominant hand horizontally over the biceps' tendon.
- Deliver a blow (slight downward thrust) with the percussion hammer to your thumb.
- Observe the normal slight flexion of the elbow and feel the biceps contraction through your thumb.
- Triceps reflex (C7-C8)
- Flex the patient's arm at the elbow, and support it in the plan of your non-dominant hand.
- Palpate the triceps tendon about 2-5cm above the elbow.
- Deliver a blow with the percussion hammer directly to the tendon.
- Observe the normal slight extension of the elbow.
- Brachioradialis reflex (C3-C6)
- Rest the patient's arm in a relaxed position on your forearm or on the client's own leg.
- Deliver a blow with the percussion hammer directly on the redius 2-5 cm above the wrist (the bony prominence on the thumb side of the wrist. *
- Observe the normal flexion and supination on the forearm. The fingers of the hand may also extend slightly.
- Planter reflex (L2-L4)
- Ask the patients to sit on the edge of the examining table so that the legs hang free.
- Locate the patellar tendon directly below the patella.
- Deliver a blow with the percussion hammer directly to the tendon.
- Observe the normal extension or kicking out of the leg as the quadriceps' muscle contract.
- Achilles reflex (ankle jerk) (S1-S2)
- With the patient in the same position as for the planter reflex, slightly dorsiflex the client's ankle by supporting the foot lightly in the hand.
- Deliver a blow with the percussion hammer directly to the Achilies tendon just above the heel.
- Observe and feel the normal planter flexion of the foot.
- Planter reflex or babinski reflex (L4-S1)
- It may be absent in the adults without pathology or overridden by voluntary control.
- Use a moderately sharp object e.g. key, dull end of pin, the handle of the percussion hammer.
- Stroke the lateral border of the sole of the patient's foot, starting at the heel, continuing towards the big toe.
- Observe the response normally all five toes bend downward; this reaction is negative babinski. In the abnormal babinski response, the toe spread outward and the big toe moves upward.
- Biceps reflex (C5-C6)
After completing procedure
- Allow the patient to put on clothes and manage.
- Explain the relevant findings to the patient.
- Replace the articles and perform hand washing.
- Record and report the important findings of physical examination.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google