Pressure Sore
Subject: Fundamentals of Nursing

Overview
Pressure Sore
Bedsores or pressure ulcers are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. It develop when pressure on the skin results in a loss of circulation, which damages the skin tissue. It is an ulcer occurring on the skin of any bed- ridden patient, particularly over bony prominences or where two skin surfaces press against each other.)
Bed sores are areas of dead tissues caused by prolonged pressure over the skin especially over bones, which cuts off the circulation so that tissues receive no nourishment.
Causes of Pressure Sores
Direct Causes
Sustained Pressure: In a bed ridden patient, constant pressure over the bony area results in poor blood circulation. This caused by occlusion of blood vessels by pressure. This results due to lack of cell nutrition and accumulation of waste materials in the cells causing cellular death or necrosis. The pressure is caused by the weight of the body continuously remaining in one position, splints, casts and bandage.
Friction: Friction of the skin with rough bedding causes injury to the skin. Friction causes friction burn that leads to sore formation. The friction is caused by wrinkles in the bed cloths, crumbs of food in the bed, chipped or rough bed pans and hard surfaces of plaster casts and splint.
Moisture: Prolonged moisture on the skin reduces the skin's resistance to trauma and can lead maceration of the skin. This may be due to excessive sweating, leaving patient lying on wet bedding, patient with incontinence of urine and stools, improper cleaning & drying of patient and careless handling of bed pans and urinals causing soiling.
Presence of Pathogenic Organisms: Due to unhygienic condition pathogenic organism multiplies and infection settles on the skin.
Sharing Force: This occurs when two surfaces are moving in opposite directions or it is the force produced when layers of tissue move on each other. Improper positioning or careless pulling or moving of the patient results in sharing force due to the pulling of skin and underlying tissue over each other. This sharing force is responsible for tearing of capillaries and arterioles resulting in poor circulation to the tissues.
Predisposing Factors
Age: The majority of pressure sores occur in people older than 70. Changes in skin and its supporting structures make the older person more prone to impaired skin integrity. This is especially true in older people who naturally have thinning skin and decreased circulation, both of which make tissue damage more likely and healing more difficult without essential nutrients carried by the blood; tissues of the skin are vulnerable to breakdown. Poor nutrition, common among older adults, not only affects the integrity of the skin and blood vessels but also hinders wound healing. These changes are generalized thinning of the epidermis, decreased strength and elasticity of the skin due to changes in the collagen fiber of the dermis, decreased vascularity of the dermis due to a reduction in the number of epithelial cells and blood vessels.
Loss of Sensory Perception: Spinal cord injuries, paralysis or other neurological disorders can results in a loss of sensation. Loss of sensation reduces a person's ability to discern injurious heat and cold and to feel the tingling, that signals loss of circulation. This loss makes the person prone to skin damage.
Poor Nutrition and Hydration: Patients are more likely to develop pressure sores if they have a poor diet, especially one deficient in protein, zinc and vitamin C. Generally, prolonged inadequate nutrition causes weight loss, muscular atrophy and the loss of subcutaneous tissue. These reduce the amount of padding between the skin and the bones thus increasing the risk of pressure sore development. Inadequate fluid intake results in skin that is dry, has decreased tissue tolerance and is less resistant to trauma.
Edema /Swelling: The presence of edema makes skin more prone to injury by decreasing its elasticity resilience and vitality. Edema increases the distance of the capillaries and cells, thereby slowing the diffusion of oxygen to the tissue cells.
Fecal and Urinary Incontinence: Problems with bladder control can greatly increase risk of pressure sores because Person's skin stays moist which promotes skin maceration and makes the epidermis more easily eroded and susceptible to injury. Bacteria from fecal matter not only can cause serious local infections but also lead to life-threatening systemic complications such as sepsis, gangrene and, rarely, necrotizing fasciitis, a severe and rapidly spreading infection.
Medical Conditions: Because certain health problems such as diabetes and vascular disease affect circulation, parts of body may not receive adequate blood flow, increasing risk of tissue damage. And if patient have muscle spasms (spastic paralysis) or contracted joints, they are subject to repeated trauma from friction and share forces.
Decreased Mental Awareness: People whose mental awareness is lessened by disease, trauma or medications are often less able to take the actions needed to prevent or care for pressure sores.
Smoking: Smoking results vasoconstriction that reduces blood flow and limits the amount of oxygen in the blood. Therefore person with smoking tends to develop bed sore and their wound heals more slowly due to lack of oxygen supply to the area.
Clients Who Are Prone to Develop Bed Sore
- Client with long term illness, fracture patients.
- Client with spinal injury.
- Paralyzed client.
- Elderly with circulatory problems.
- Obese client.
- Edematous client.
- Very thin client.
- Sedated client.
- Malnourished client.
- Client with incontinence.
Common Sites Liable to Get Bed Sore
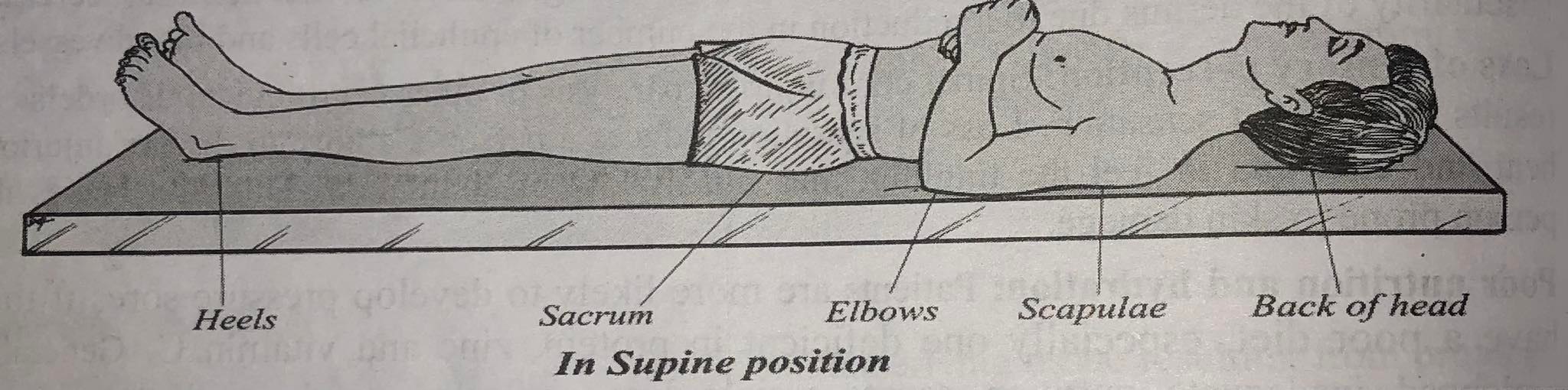
Pressure sore usually occurs over bony prominences. These areas do not have much subcutaneous fat to protect the skin tissue from the pressure of the body weight. Bony pressure areas are: In supine position: occiput, scapula, sacral region, elbow, heels.
In Supine Position: occiput, scapula, sacral region, elbow, heels.
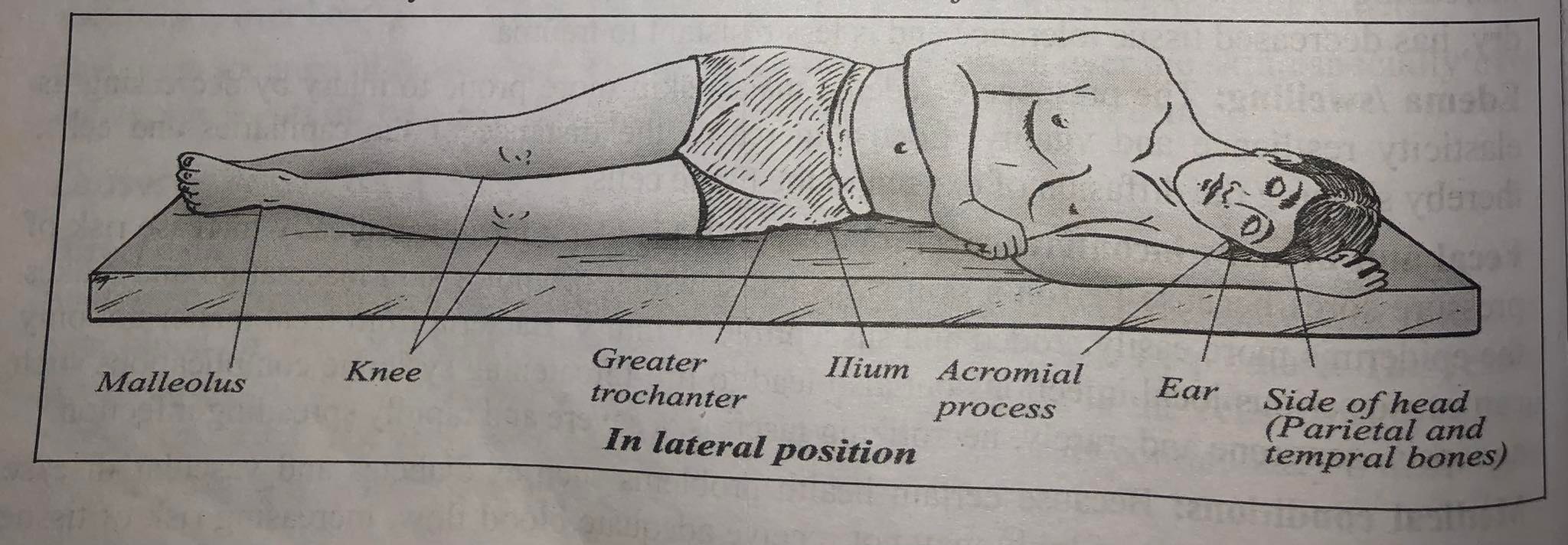
In Side Lying Position: Ears, acromion process of shoulder ribs, greater trochanter of hips, medial and lateral condyles of knee and malleolus of ankle joint.
In Prone Position: Ears, cheeks, acromion process, breast in female genitalia in male, knees, toes.
_1671509057.jpg)
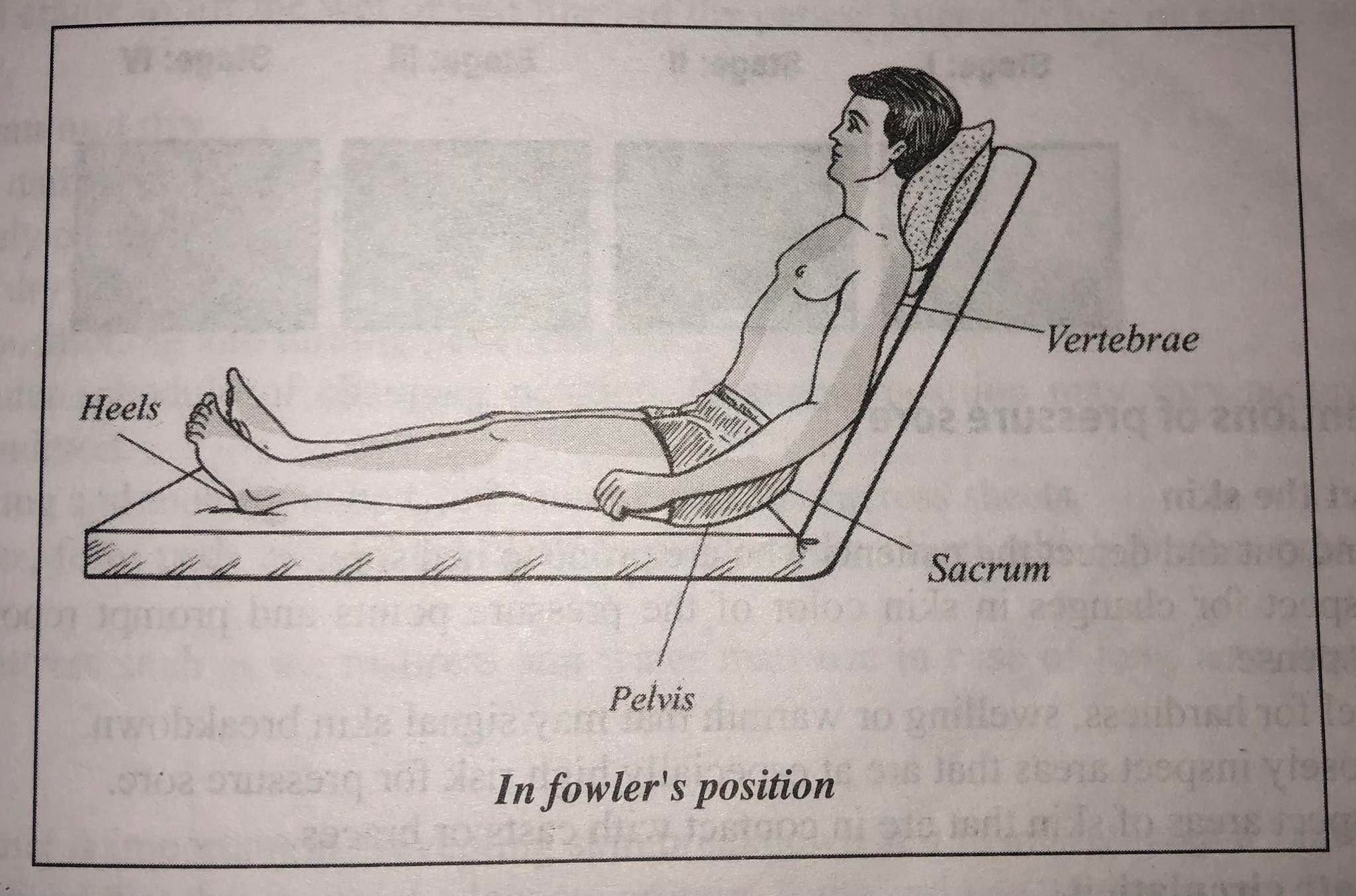
In Fowler's Position: Vertebrate, sacrum, pelvis, heels.
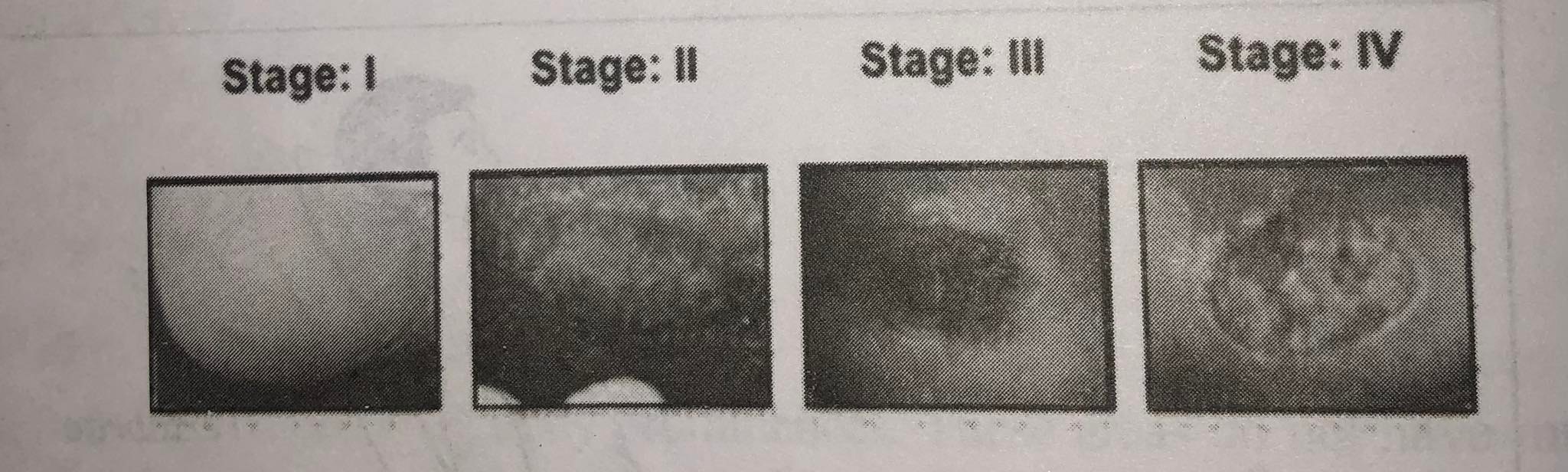
Degree of Pressure Sores Based on Clinical Manifestation
Based on the severity of the condition, bed sores go through four different stages and the symptoms seen during each stage vary.
1st Degree
- The skin remains intact. Its color may remain differ from the surrounding area.
- The skin is red, tender and inflamed usually over a bony prominence.
- The area differs in characteristics such as pain, softness, tenderness and change in temperature around the skin
- A Stage one bedsore is a warning to caregivers and/or family members because bedsores develop quickly and progress rapidly.
2nd Degree
- Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound.
- The skin is blue or mottled, insensitive, circulation cut off and gangrene develops.
- Loss or damage in the underlying layer of the dermis as well as the epidermis
- Appearance of pinkish, shallow and basin-like wounds
- Ruptured fluid-filled blisters on the skin
- Once a bedsore gets past this stage it becomes much harder to treat.
3rd Degree
- Full thickness skin loss involving damage to or death of, the subcutaneous tissue that may extend down to, but not through, underlying connective tissue (fascia).
- Development of deep wound at the site of the ulcer.
- The wound will look like a fairly deep crater, black at its edges.
- Stage three bedsores are powerfully sad and visually disgusting.
4th Degree
- Full thickness skin loss with extensive destruction, tissue death, and/or damage to muscle, bone, or supporting structures (e.g., tendon, joint, capsule).
- They will look like a large, deep, open wound revealing bone and connective tissue.
Preventions of Pressure Sore
Inspect the Skin
- Find out and detect the patients who are prone to bed sore.
- Inspect for changes in skin color of the pressure points and prompt reporting in case of suspense.
- Feel for hardness, swelling or warmth that may signal skin breakdown.
- Closely inspect areas that are at especially high risk for pressure sore.
- Inspect areas of skin that are in contact with casts or braces.
Stimulate Circulation
- Massage the skin especially to pressure area.
- Clean area regularly
Relive Constant Pressure
- Position should be changed at least every 2 hours.
- Give bed pan carefully.
- Use special mattress, beds and comfort devices such as earrings, pillows.
- Loose tight bandages and restrains.
- Pad pressure points inside plaster casts.
- Early ambulation of the patient.
Prevent from Friction of Skin
- Provide a smooth firm and wrinkle free bed.
- Keep the bottom clothes free from crumbs and foreign bodies.
- Apply pads to parts of the body which rub against each other.
- Pad pressure points inside plaster casts, splint.
- Special care should be taken during patient's urination and defecation to prevent soiling of bed linens.
Prevent Moisture
- Handle bed pans and urinals carefully to prevent soiling.
- Change linen when it is wet or soiled.
- Wipe off perspiration and keep patient dry.
- Give care to patient immediately following of micturition and defecation.
- Insert self-retaining catheter with incontinence of urine.
Prevent Skin Injury
- Cut the nails of both nurse and patients short.
- Take special care while giving and removing bed pan to avoid scratching skin.
- Help should be taken while moving heavy & difficult patient.
- Avoid mechanical or physical injury to the skin from improper fitting of prosthesis or from burns caused by excessively hot or cold applications.
- Use a bed cradle to lift the wet of bed linen of the patient to enable him or her to move in bed freely.
Keep Skin Clean and Dry
- Give bath daily with mild soap and rinse and dry thoroughly.
- Immediately change linen when it is wet or soiled.
- Wash and dry skin after any leakage of stool or urine.
- Padding, positioning and turning patient in bed audi
- Make regular schedule of changing position. Changing position may vary according to client's condition.
- When turning and moving in bed, left rather than slides across sheets.
- Use pillows, form pads and folded cloth to position the client which protect pressure on bony areas
- Special mattress such as air mattress and water matt use in case of long term bed ridden clients.
Nutrition
- A healthy diet is important in preventing skin breakdown and in aiding wound healing.
- Give a balanced diet that includes adequate protein, fruits and vegetables.
Lifestyle Changes
- Learn for most effective way to stop smoking. Tobacco use decreases oxygen to skin.
- Daily exercise improves circulation, builds up vital muscle tissue, stimulates appetite and strengthens body overall.
Support - Physical and emotional well-being depend on having a strong support system.
Management of Patient with Pressure Sore
1st Degree
- Detect the early signs and symptoms of bed sore and report them to the sister in charge and the doctor.
- Carry out all the preventive measures with special care to prevent extension of bed sore and further occurrence of pressure sores.
- While giving back care, do not over the reddened or inflamed area itself but start just outside the affected area and move outwards in a circle using circular motion.
- Consult for further treatment.
- Use mechanical devices e.g. air ring, water mattress.
2nd Stage
- Inform and report to the senior.
- Prevent the ulcerated areas from infection.
- Use normal saline for cleaning the area.
- If sloughing is more; clean the wound twice daily cut off slough.
- Apply heat for healing of the wound. Use 100 watt electric bulb for 10 minutes.
- Use mechanical devices.
3rd and 4th Stage
- Inform and report to the ward sister.
- To treat infection, apply soframycine ointment locally and give systematic antibiotics after culture and sensitivity test.
- Provide nutritious diet, sun light and fresh air.
- If slough is present, clean the wound twice daily. If the slough is loose, may be cut off.
- If there is delay in wound healing, skin grafting can be done.
Treatment of Pressure Sore
Treating bedsores is challenging which is why prevention is the best treatment. Open wounds are slow to close, and because skin and other tissues have already been damaged or destroyed, healing is never perfect.
Conservative Treatment: Although it may take some time, most Stage I and Stage II bedsores will heal with conservative measures. The first step in treating a bedsore at any stage is relieving the pressure that caused it. Changing positions in bed often reduces pressure on any one spot. Caregivers need to follow a schedule for turning and repositioning.
Using support surfaces such as special cushions, pads, mattresses and beds that relieve pressure on an existing sore and help protect vulnerable areas from further breakdown.
It is essential to keep wounds clean to prevent infection. A stage I wound can be gently washed with water and mild soap, but open sores should be cleaned with a saltwater (saline) solution each time the dressing is changed.
Avoid antiseptics such as hydrogen peroxide and iodine, which can damage sensitive tissue and delay healing.
Debridement: The removal of damaged tissue (debridement) is a necessary but painful way to repair Stage II and higher bedsores. To heal properly, these wounds need to be free of damaged, dead or infected tissue.
Aggressive/surgical Treatment: Even with the best medical care, once bedsores get started they can quickly reach a point where they require surgical intervention. Most bedsores are repaired using a pad of muscle, skin or other tissue that covers the wound and cushions the affected bone (flap reconstruction). The tissue is usually harvested from a healthy area of patient's body.
Complications from Pressure Sore
Cellulitis: This acute infection of skin's connective tissue causes pain, redness and swelling, all of which can be severe. Cellulitis can also lead to life-threatening complications, including sepsis and meningitis - an infection of the membrane and fluid surrounding your brain and spinal cord.
Bone and Joint infections: These develop when the infection from a bedsore burrows deep into joints and bones. Joint infections (septic or infectious arthritis) can damage cartilage and tissue within days, whereas bone infections (osteomyelitis) may fester for years if not treated. Eventually, bone infections can lead to bone death and reduced function of joints and limbs.
Necrotizing Fasciitis: This rapidly spreading infection destroys the layers of tissue that surround your muscles. Initial signs and symptoms include fever, pain and massive swelling. Without treatment, death can occur in as little as 12 to 24 hours.
Gas Gangrene (myonecrosis): A rare and severe form of gangrene, myonecrosis develops suddenly and dramatically and spreads so rapidly that changes in tissue are noticeable within minutes. The clostridium bacteria responsible for gas gangrene produce toxins that completely destroy affected muscle tissue and cause potentially fatal systemic problems.
Amputation: When left untreated bedsores will continue to fester and destroy live tissue. If left unchecked long enough it will manifest in the bone. This then leads to the need to amputate a limb (usually a leg) to stop the spread of the deeply burrowed wound.
Sepsis: One of the greatest dangers of an advanced pressure sore is sepsis occurs when bacteria from a massive infection enter bloodstream and spread throughout your body - a rapidly progressing, life-threatening condition that can cause shock and organ failure.
Cancer: This is usually an aggressive carcinoma affecting the skin's squamous cells. It often can spread to the lymph nodes by the time it's diagnosed.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google