BACTERIOLOGY
Subject: Basic Science Applied to Nursing

Overview
Introduction to Bacteriology
-
Prokaryotic, unicellular microorganisms make up bacteria. A microscope is needed to investigate their morphology.
-
Bacteria can have either an autotrophic (capable of producing their own food) or a heterotrophic method of nutrition (depends on other organisms for nutrition).
-
By using binary fission, which involves a single-celled bacteria dividing into two identical daughter cells, they can reproduce.
-
Size: 0.5 to 15 mm in length; 0.2 to 2 mm in width
Classification of bacteria
Bacteria can be classified on the basis of following things:
-
Shape
-
Arrangement
-
Temperature requirement and
-
Oxygen requirement
Bacteria are grouped according to shape as:
-
Cocci
-
Bacilli
Spirochetes
Actinomycetes
Mycoplasmas
Ricketssiae and Chlamydiae
Based on the arrangement of the flagella:
-
Monotrichous
-
Lophotrichous
-
Amphitrichous
-
Peritrichous
Based on the required temperature:
-
Psychrophilic bacteria
-
Mesophilic bacteria
-
Thermophilic bacteria
Based on the need for oxygen:
- Aerobic bacteria
- Anaerobic bacteria
- Microaerophilic bacteria
Nutritional Requirements of Bacteria
A few necessary elements for healthy bacterial growth include:
- Water:
As a source of hydrogen and oxygen, water is necessary. Water makes up about 80% of bacterial cells, which is a crucial component for their ability to grow. - Carbon:
Carbon is the central component that synthesizes every organic compound. Carbon is an essential factor to nourish bacteria. Bacteria get carbon by the breakdown of organic compounds such as carbohydrate, proteins or directly in form of CO2. - Hydrogen:
Hydrogen is also a key component to provide nutrition to the bacteria. It participates in the energy generation processes in most microorganisms. - Oxygen:
Oxygen is required for respiration by many microorganisms; mainly for aerobic microorganisms (aerobic bacteria). Bacteria get oxygen either from H2O or organic compounds or directly in O₂ form. - Nitrogen:
It is a major component of protein and nucleic acid and its main source is ammonia. Nitrogen is available to bacteria either from the environment or may be produced by the deamination of amino acids by bacteria. - Inorganic sources:
Inorganic elements required for bacterial growth are: Phosphorus,Sulphur, Potassium, Magnesium, Calcium, Iron, Copper, Zinc. These are required for enzyme function. - Organic growth factors:
Some bacteria require organic compounds for their growth. These are also called as bacterial vitamins. eg. Haemophilus influenzae require haemin and NAD (nicotinamide adenine dinucleotide) for growth. - Temperature:
For growth of different bacteria optimum temperature is different. The majority of pathogenic bacteria grow in the range of 20-40°C. - pH or Hydrogen ion concentration:
The optimum pH necessary for growth of most pathogenic bacteria is in between 7.2-7.4 (similar to physiological pH of man). However, Lactobacilli and Thiobacillus grow at acidic pH of 3 while Cholera vibrios and Alkaligenes grow at alkaline pH of 10.5 - Light:
Phototrophic organisms require light in order to carry out photosynthesis, where as other bacteria prefer to grow in darkness.
Bacterial Division
Bacteria divide mainly by binary fission and by other forms of reproduction.
-
Binary Fission:
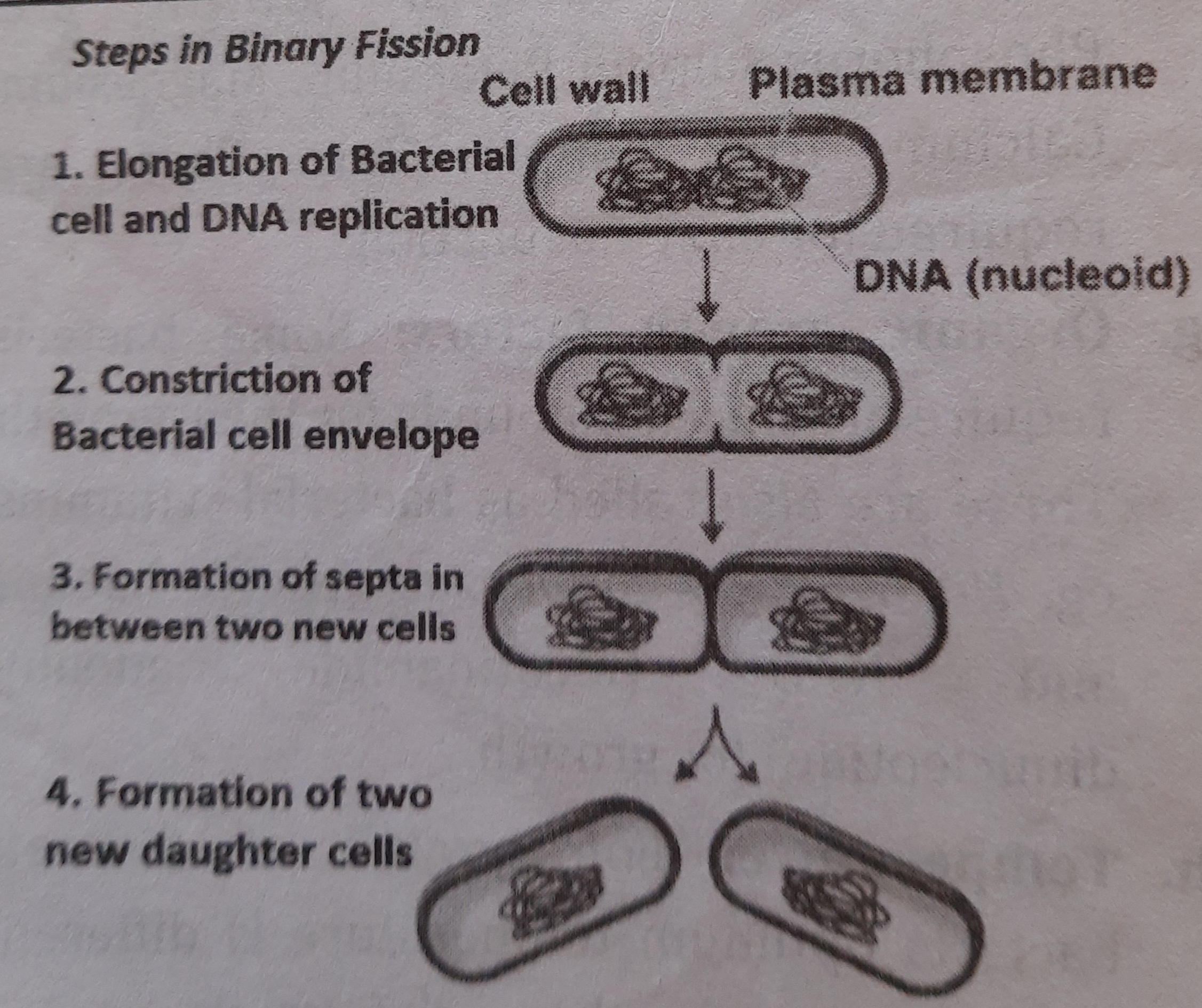
Bacterial cells generally reproduce by a process of binary fission. It is a type of reproduction in bacteria (prokaryotes) where a bacterial cell is divided into two identical cells. (fission means dividing or splitting). Following processes occur in binary fission:-
Elongation of bacteria: bacterial cell elongates and DNA replicates. Thus produces two daughter DNA which moves to the two ends of bacteria.
-
Constriction of cell envelope: Cell wall and cell membrane constrict. Afterwards, a septum is formed which divides the cell into two.
-
Formation of two daughter cells: After the septum is complete, two identical daughter cells are formed.
-
-
Other Unusual forms of Reproduction:
-
Budding: In some bacteria only, reproduction occurs by budding. In this process a small bud forms at one end of the mother cell or on filaments. When the bud is enlarged and is about the same size as the mother cell, it separates. eg. Planctomyces species, Caulobacter, Hyphomicrobium etc.reproduce budding. by
-
Baeocyte production: Baeocyte literally means small cell. A small cell starts out from the original cell which begins to grow in size. Cellular DNA also undergo replication for many times which later on produce a number of baeocytes. eg. Stanieria reproduce by Baeocyte formation.
-
Bacterial Growth Curve
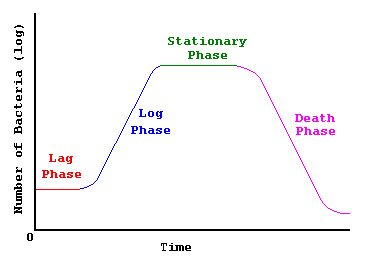
Bacterial growth is regulated by nutritional environment. When bacteria are inoculated in a suitable liquid medium, bacterial growth occurs. Bacterial growth leads to an increase in the number of bacterial cells. The growth curve has got four main phases:
-
Lag phase:
When bacterium is inoculated in a culture medium, they undergo a period of adaptation called lag phase. During this phase necessary enzymes and intermediates a^ prime n * 5na*psi are synthesized. Size of bacteria is increased Same but number remains constant. The time taken by lag phase varies but on an average it is around 1-4 hours (average 2 hours) -
Log phase:
During this phase, cell division proceeds and bacterial number increase exponentially. There occurs maximal rates of cell division in this phase. Average us phase pircine suration rachu duration is 8 hours. -
Stationary phase:
There is slow rate of cell death which is compensated by the formation of new cells through growth. After some time, bacterial growth stops almost completely due to depletion of nutrients or accumulation of toxic products. -
Death phase or decline phase:
Number of bacterial cells decreases in this phase due to death of bacterial cells. Sometime, small number of cells may survive even after death of majority of cells. The survivors may take nutrients from the dead cells.
Bacterial Cell Anatomy
The structure of bacteria contains following components:
- The outer layer or cell envelope: it consists of :
- A rigid cell wall
- Plasma membrane / Cytoplasmic membrane
-
Cytoplasm: It consists of mesosomes, ribosomes, intracytoplasmic inclusions
-
Nucleus
-
Bacterial capsules
-
Flagella
-
Fimbriae
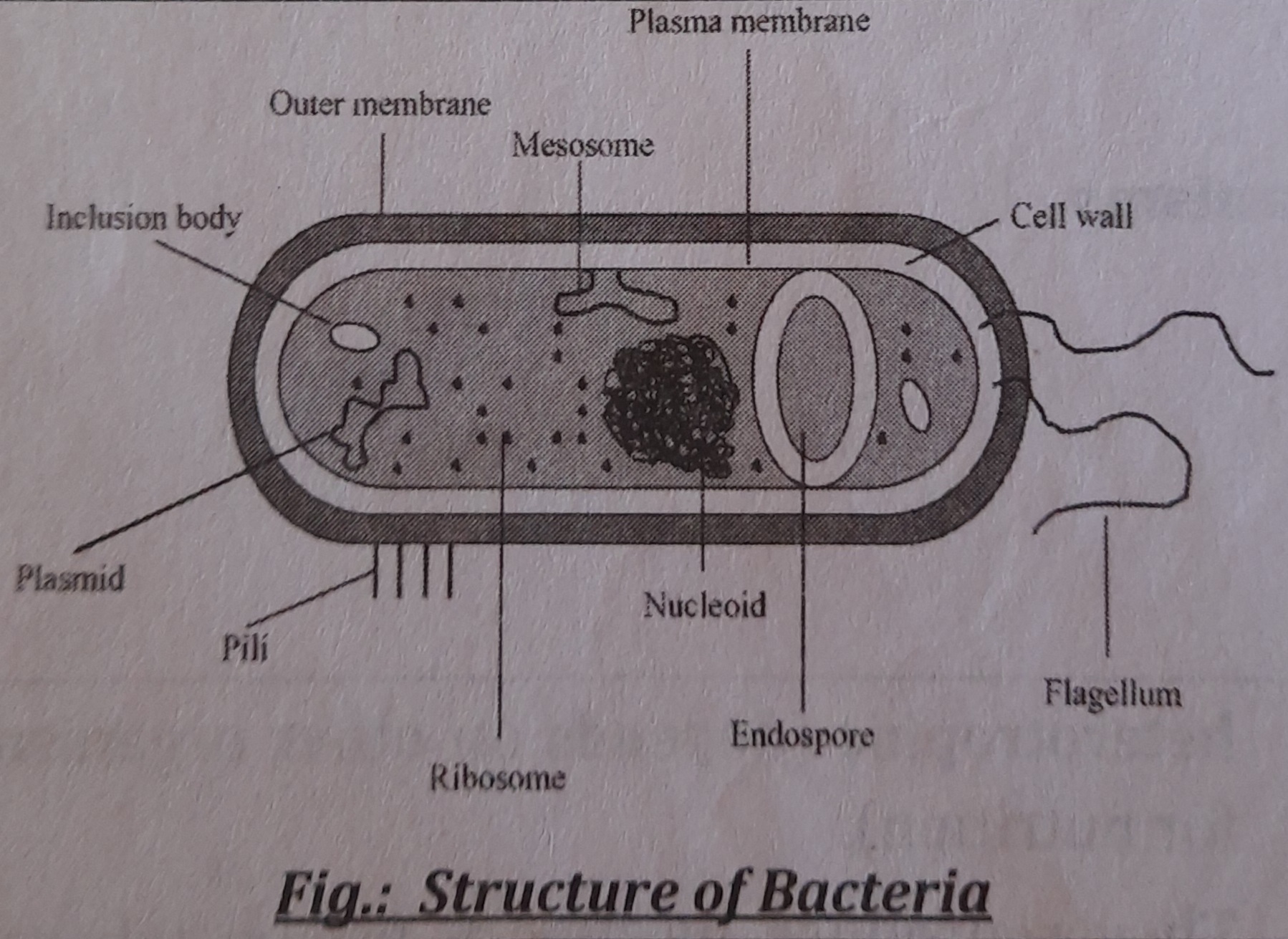
1. The Cell wall
The cell wall encloses a bacterial cell is a strong and rigid structure. It contributes roughly 20–25% of the dry weight of the cell. Since it is porous and elastic, solute molecules can move freely through it. A peptidoglycan comprised of N-acetylglucosamine and N-acetylmuramic acid molecules is what gives the cell wall its stiffness. The cell walls of gram positive bacteria are less complex chemically than those of gram negative bacteria.
-
Gram negative cell wall:
The gram negative cell wall has the following components:-
Lipoprotein layer: It connects the peptidoglycan to outer membrane
-
Outer membrane: It contains specific proteins such as outer membrane protein (OMP).
-
Lipopolysachharides: It consists of lipid A, to which a polysachharide is attached. The toxicity of bacteria is associated with lipid A. The periplasmic space: It is the space between the inner and outer membrane.
-
Peptidoglycan: It is 2 nm thick in gram negative bacteria.
-
-
Gram-positive cell wall:
The followings are the components of gram positive cell wall:-
Peptidoglycan: It is 16-80 nm thick in gram positive bacteria
-
T-eichoic acid: It is present in significant amount in gram positive bacterial cell wall but absent in gram negative bacteria. It constitutes major surface antigens of gram positive bacteria.
-
Other components: Some gram positive bacteria also contain antigens such as protein and polysachharides.
-
-
Functions of cell wall:
The bacterial cell wall performs following functions:-
It accounts for the shape of the cell.
-
It provides protection to the cell.
-
It provides rigidity to the bacterial cell
-
It takes part in cell division
- It possesses target site for antibiotics, lysozymes and bacteriophages. It carries bacterial antigens which are important in virulence and immunity.
-
| Character | Gram positive bacteria | Gram negative bacteria |
|---|---|---|
| Thickness | Thicker | Thinner |
| Periplasmic space | Absent | Present |
| Lipids | Absent or small amount | Present |
| Teichoic acid | Present | Absent |
| Peptidoglycan | 16-80 nm thick | 2 nm thick |
2. Cytoplasmic membrane
It is a semipermeable layer which lies beneath the cell wall. It is 5-10 nm thick. It is made up lipids and proteins.
Functions:
-
It is the site of various enzymes such as permease, oxidase, polymerase which are involved in active transport of nutrients.
-
It contains the enzymes required for cell wall synthesis.
-
It acts as an osmotic barrier.
3. Cytoplasm
It is a viscous watery solution that contains a variety of organic and inorganic compounds. It doesn't contain mitochondria and endoplasmic reticulum. It contains:
-
Ribosomes: These are the sites of protein synthesis. They are 10-20 nm in size with a sedimentation coefficient of 70 S (S= svedberg unit)
-
Mesosomes: These are invaginations of plasma membrane into the cytoplasm. They contain respiratory enzymes and are responsible for ATP production.
-
Intracytoplasmic inclusions: These are sources of stored energy and are present in some species of bacteria.
4. Nucleus
A narrow double-stranded DNA helix tightly coiled inside the cytoplasm makes up the bacterial nucleus. Nuclear membrane and nucleolus are absent. Some bacteria may have DNA-based extranuclear genetic material, sometimes known as plasmids or episomes, in their cytoplasm. Bacterial traits like toxigenicity and drug resistance are determined by the plasmid.
5. Bacterial capsule
The bacterial cell wall is encased in a thick, jelly-like substance on the outside. It has a thickness of roughly 0.2 m. It has 2% solids and practically all of it is water. Normally, it is a polysachharide, however in some bacteria, it is a polypeptide (such as in anthrax bacillus). Streptococcus pneumonia, Klebsiella species, Bacillus anthracis, Hemophilus influenza, and Cryptococcus neoformans are among the organisms in capsules.
Some of the functions of capsule are:
-
It enhances bacterial virulence by inhibiting phagocytosis.
-
It acts as protective covering that prevents bacteria from bacteriophages, phagocytes, enzymes.
-
Capsules contain specific type of antigen and can be used for identification and typing of bacteria.
6. Flagella
They are cytoplasmic extensions that are filamentous and protrude through the cell wall. They are made of the protein Flagellin and have an unbranched, lengthy, threadlike structure. They have a diameter of 0.01-0.02 m and a length of 5 to 20 m. 10 to 20 can be found in each compartment.
Parts of flagella: each flagellum has three parts:
-
Filament
-
Hook
-
Basal body
The hook and filament are joined at the cell surface from outside the cell. The cell envelope contains the hook-basal body section. The inner and outer rings of the basal body are what bind it to the cytoplasmic membrane.
There are a few different arrangements/types of Flagella. Flagella are arranged on bacterial body in the following ways:
- Monotrichous: single flagellum at one end eg. Vibrio cholera
- Amphitrichous: C. single flagellum at both ends. Eg, Alcaligenes faecalis Lophotrichous: tufts of flagella at one or both ends. Eg, Spirilla
- Peritrichous: flagella arranged all around the bacterial cell. Eg. Salmonella typhi.
Flagella serve as the organs's means of locomotion.
7. Fimbriae/Pili:
They are straight filaments that emerge from the cell surface like hair-like appendages. They are less than 10 nm thick and range in length from 0.1 to 1 m. Some gram negative bacteria contain them. There are 100–500 fimbriae peritrichously in each bacteria. Pilin is the name of the protein that makes them up.
There are three main types of fimbriae, they are:
-
Common pili
-
Sex or F(fertility) pili
-
Coll (colicin) pili
A few functions of fimbriae are as follows:
-
They are the organs of adhesion
-
Sex pili are found on male bacteria. They help male bacterial cell to attach with female bacterial cells in forming conjugation tubes through which genetic material is transferred to female cells.
BACTERIAL SPORES
They are a highly dormant stage of bacteria that develops under harsh circumstances like hunger and desiccation. Each vegetative cell produces one spore during the sporulation process, and each spore produces just one vegetative bacteria during germination. All medically significant bacteria's spores are killed by autoclaving for 15 minutes at 121 °C.
Morphology of spore:
As nuclear chromatin condenses to create the forespore, the transparent region of the cell protoplasm gradually darkens. The spore wall is formed by the cell membrane growing inward toward the core (forespore). The spore membrane, from which the cell wall of the ensuing vegetative bacteria develops, is formed by the innermost layer of the spore wall. A dense layer of spore cortex is present outside of this membrane, and it is encircled by a multilayered spore coat. Exosporium is the name for a loose outer layer that some spores have.
Spore forming bacteria:
Bacillus anthracis, Bacillus subtilis, Clostridium tetani, Clostridium welchii, and Clostridium botulinum are the microorganisms (bacteria) that produce spores.
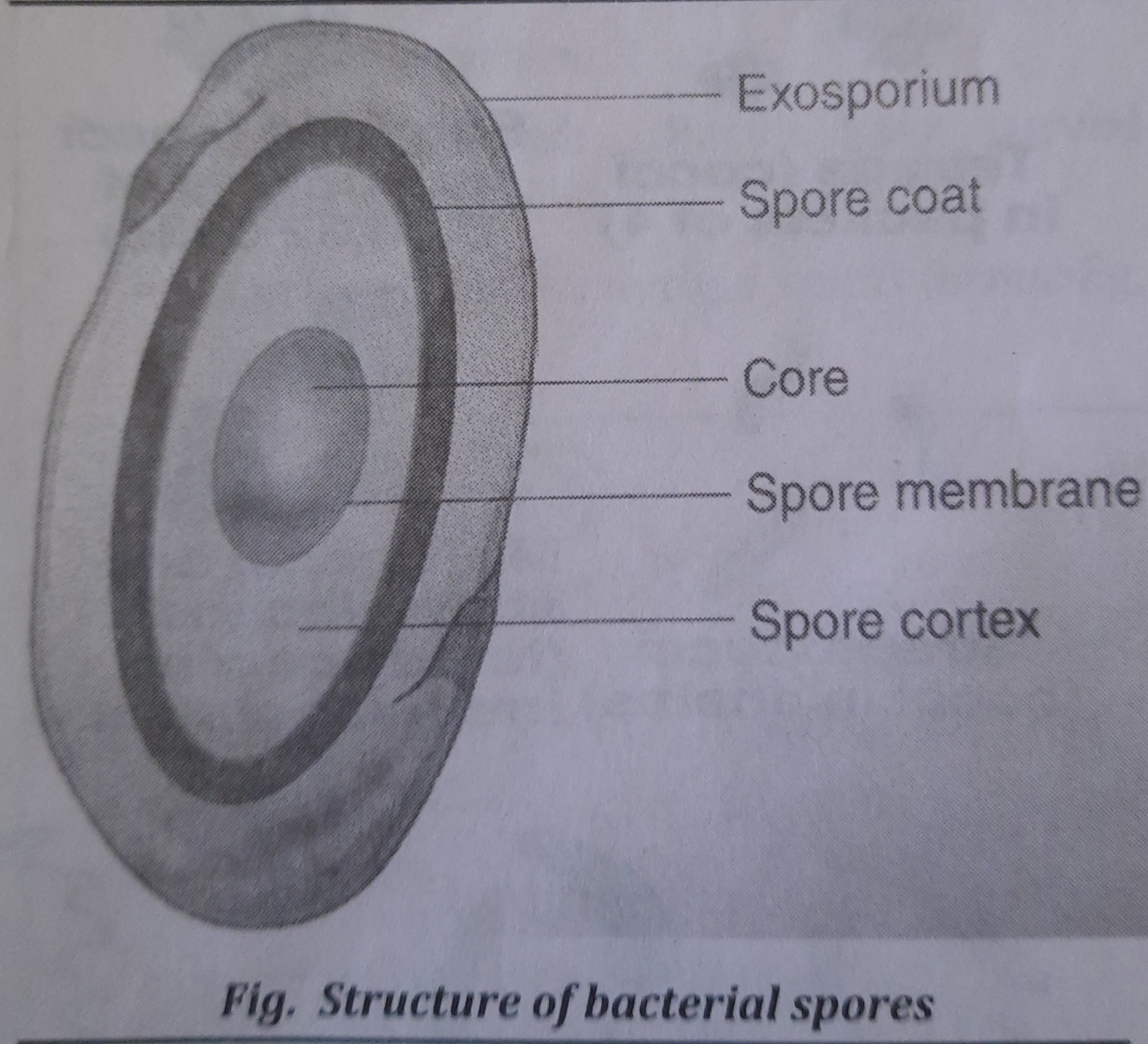
Uses of spores
Spores of specific bacterial species are used as a gauge for effective sterilization. For instance, during autoclaving, Bacillus stearothermophilus spores are utilized as an indication.
Culture Media
The preparation of nutrients or food used to cultivate microorganisms in a lab is referred to as a culture medium. For diagnostic reasons, culture medium is created to identify pathogenic bacteria and conduct an antibiotic susceptibility test. Examples of culture media include potato dextrose agar, nutrient broth, and nutrient agar.
Composition of media
Culture medium is composed of different nutrients and other factors that are essential for a microbial growth. Culture media contain a variety of factors which ultimately help for growth of microorganisms. These are water, sodium chloride, peptone, meat extract, mineral salts (e.g. sulphates, phosphates), a suitable pH (pH * (7.2 - 7.4)) , blood, agar, accessory growth factors, antibiotics etc.
Basic constituents of culture media are:
-
Nutrients: These are sources of carbon, nitrogen, energy, inorganic and organic constituents, electrolytes such as sodium chloride etc. Besides, other ingredients of culture media are peptone, meat and yeast extract, blood etc.
-
Water: water is a source of hydrogen and oxygen.
-
Agar: It acts merely as a solidifying agent and does not provide any nutrition to the bacteria. It contains mainly carbohydrate (complex polysaccharide), a small amount of protein like material and sometimes traces of long chain fatty acids.
Types of media
Culture media can be broadly classified on the basis of:
-
Physical state
-
Solid culture media
-
Semisolid culture media
-
Liquid culture media
-
-
Utility purpose
- Basal media
- Enriched media
- Enrichment media
- Selective media
- Differential media
- Transport media
- Biphasic media
Staining Techniques
Staining
Microorganisms are colored using chemicals or dyes using the staining procedure on a fixed smear. The bacteria can be seen thanks to staining procedures. Colored chemicals (dyes) add color to the cells or cell components during staining operations.
Smear techniques
-
Smear technique consists of spreading a thin film of liquid suspension of cells on a slide.
-
The smear made from bacterial cultures (specimens) are dried in air, and are heat fixed by passing the slide through flame.
-
Finally, the heat fixed smear is stained by appropriate dyes and can be seen through microscope.
Different types of stains are possible to stain bacteria they are as follows:
-
Simple stains: Solution of single basic dye such as methylene blue or basic fuchsin are used as simple stain.
-
Negative stain: When bacteria are mixed with dye, the background is stained but bacteria remains contrastingly colorless. It is useful in demonstration of bacterial capsule.
-
Differential stains: These stains impart different colors to the different bacteria or their structures. Two commonly used differential stains are Gram's stain and Acid-fast stain.
Gram's Stain
In medical bacteriology, it is the stain that is most frequently utilized. The Danish bacteriologist Christian Gram is credited with developing the staining method that was used to identify germs in tissues.
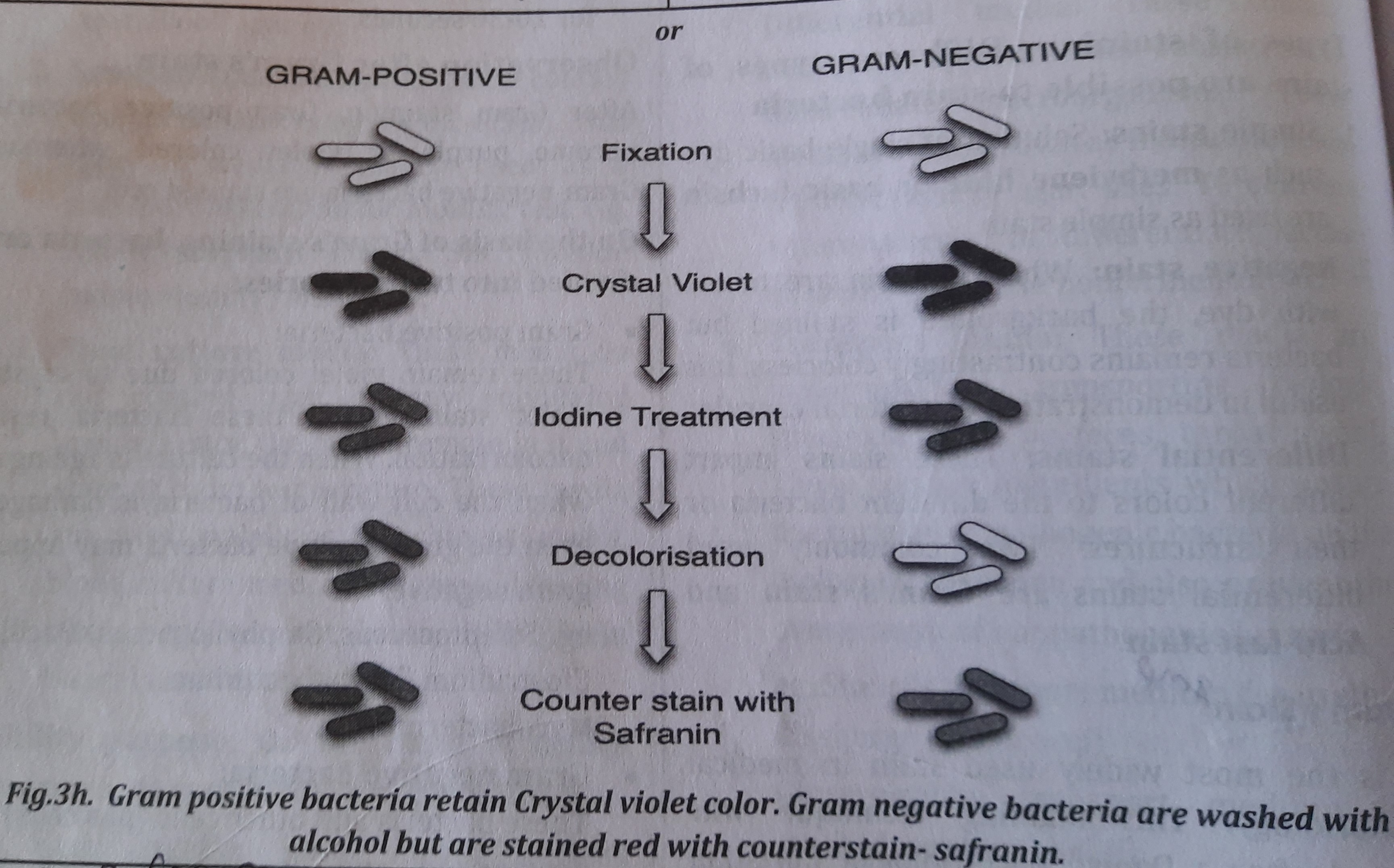
Principle of Gram's stain:
When treated with crystal violet and iodine, the bacteria smear that had been air dried and fixed by heat takes on stain and appears purple. The staining reaction between the dye (crystal violet) and the cellular interior of bacteria is accelerated by iodine. The alcohol or acetone treatment decolorizes gram negative bacteria and counterstaining with safranin, stains gram negative bacteria red. However, gram positive bacteria retain purple color (color of crystal violet).
The steps followed in this technique are:
-
Heat fixed smear is stained with a dye, such as crystal violet or gentian violet- for one minute.
-
Dilute iodine solution is poured and kept for one minute.
-
The smear is washed with water and is decolorized with alcohol or acetone- for 10 to 30 seconds.
-
The smear is washed with water and is counterstained with safranin or neutral red- for 20-30 seconds.
Observation after Gram's stain:
After Gram staining, Gram-positive bacteria become purple or violet colored whereas, Gram-negative bacteria are stained red.
On the basis of Gram's staining, bacteria are divided into two categories:
- Gram positive Bacteria:
Due to crystal violet staining, these retain their violet tint and don't fade easily. Even gram positive bacteria may appear gram negative if the culture is old or if the bacteria's cell wall is broken. Staphylococcus, Bacillus, Clostridium, Corynebacterium, Mycobacterium, etc. are a few examples.
- Gram negative Bacteria:
These bacteria and other cells (pus cells) are decolored and counterstained pink. such as Shigella, Neisseria, Vibrio, and Salmonella.
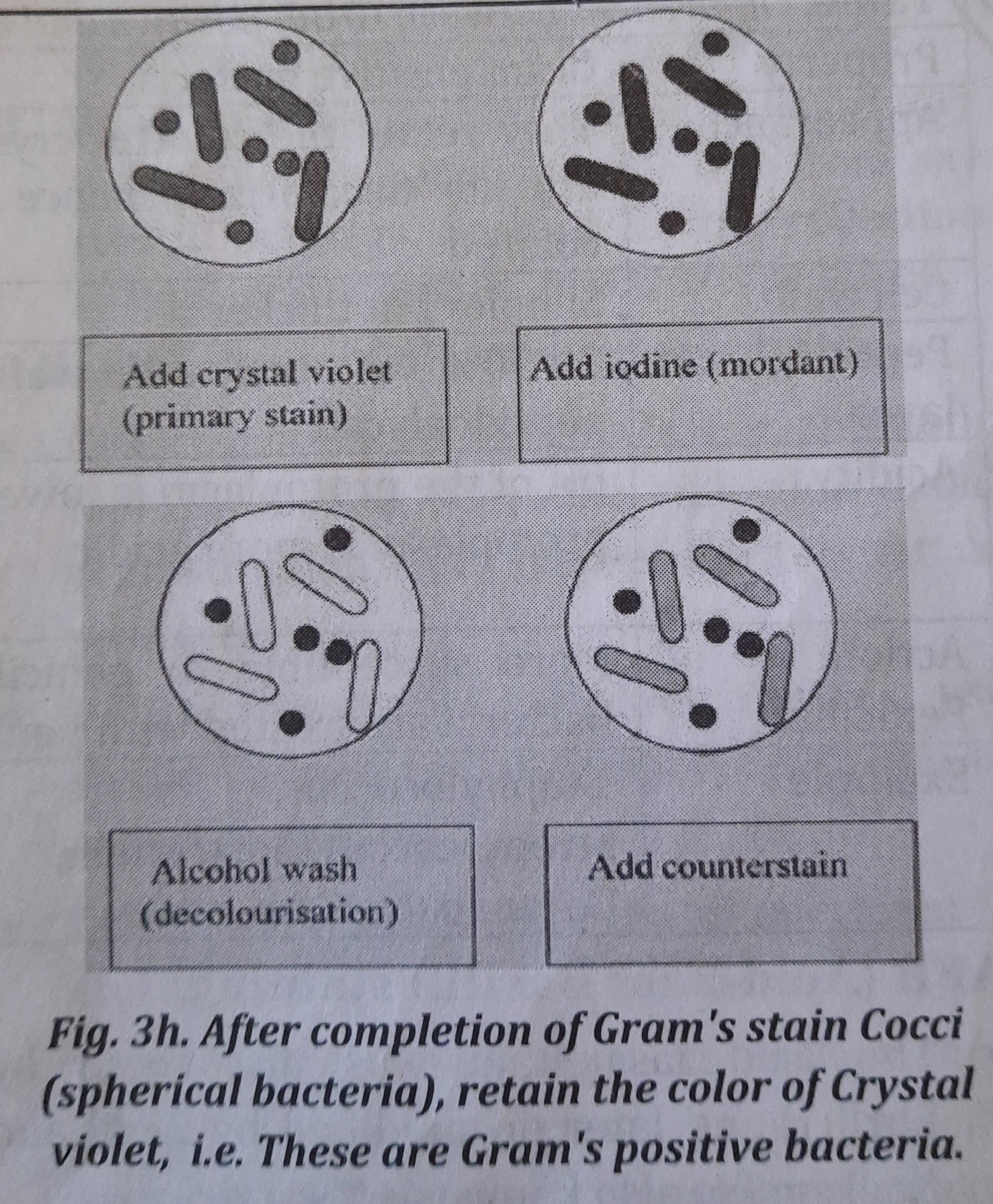
Bacilli, which are rod-shaped bacteria, are decolored (washed with alcohol) once Gram's staining is complete, and then they are once more stained with counterstain (with safranin).
| Property | Gram positive bacteria | Gram negative bacteria |
|---|---|---|
| Appearance | They retain the color of crystal violet and are not decolorized, hence appear violet colored | They are decolorized and counter stained by safranin, hence appear red coloredie |
| Cell wall | Simpler but thicker | Complex but thinner |
| Peptidoglycan layer | 70-90% of the cell wall consists of peptidoglycan | Only 10-30% of the cell wall consists of peptidoglycan |
| Acidity | pH of the protoplasm is lower (pH 2-3), i.e. protoplasm is more acidic. | pH of the protoplasm is higher (pH 4-5), i.e. protoplasm is less acidic. |
| Action of Penicillin | More susceptible to penicillin, i.e. these bacteria are treated with penicillin. | Not susceptible susceptible to penicillin or less |
| Example | Staphylococcus, Streptococcus, Clostridium, Corynebacterium etc. | Vibrio, Neisseria, Branhamella, Salmonella, Escherichia coli, Proteus species etc. |
AFB (Acid-Fast Bacilli) staining
-
The acid fast stain was discovered by Ehrlich and later on modified by Ziehl and Neelsen (so also known as ZN stain).
-
It is difficult to stain Mycobacteria with ordinary stain (Gram's stain), so this staining technique was developed.
-
Acid fast bacteria have high content of lipids, fatty acids and higher content of alcohols. Mycolic acid is found in all acid fast bacteria.
-
Acid-Fast organisms: eg. Mycobacterim- Mycobacterium tuberculosis, Mycobacterium leprae. Others- Bacterial spores, Some Nocardia species and Cryptosporidium spores.
Principle of acid fast stain:
Strong binders of carbol fuchsin, such as Mycobacterium TB and Mycobacterium leprae, resist destaining by decolorizing agents such strong acids. When exposed with acid solution, acid fast negative bacteria (other bacteria) quickly remove the stain. The decolorized acid-fast negative bacteria and other cells take on a blue hue after being counterstained with methylene blue (or malachite green), in contrast to red-colored acid-fast organisms.
Procedures:
-
Fixed smear is stained with hot carbol fuchsin- for 10 minute and is washed in tap water.
-
The smear is decolorized by 1% Hcl in 70% alcohol or by 20% Sulphuric acid- for half to one minute.
-
The smear is couterstained with 2% methylene blue or malachite green- for 2 minutes and washed in water.
Identification of Acid-Fast bacteria:
After completion of AFB staining, Acid-Fast Bacilli appear Red.
COLLECTION AND TRANSPORT OF SPECIMEN FOR IDENTIFICATION OF COMMON BACTERIAL COMMUNICABLE DISEASES
Standard Safety Precautions
The health professional should take his/ her safety precaution to be free from infection from exposure to clinical specimens. To take safety precaution following measures should be taken:
-
Personal protective measures: such as wearing gowns, aprons, gloves, mask, or goggles where required.
-
Handling of clinical specimens: Care should be taken not to touch specimen with bare hand, instead wear gloves that are impermeable to liquids and change them between every patient. Similarly, syringe and needles should be disposed properly in a puncture resistant, autoclavable discard container and try not to recap any needle.
-
Work practice: Working area in laboratory should be clean enough to be free from any kind of infection. Besides, for the collection of appropriate sample, practice is required.
A Knowledge on Collection of Specimen
-
Collect culture specimens before antibiotic therapy. During specimen collection avoid contamination from normal flora as far as possible.
-
Utilize appropriate collection devices, use sterile equipment and aseptic technique to collect specimens.
-
Collect an adequate amount of specimen in sturdy, sterile, leak proof containers.
-
When patients must have to collect their own specimens, clear and specific instructions on proper collection techniques must be given to them.
-
After collection, the specimen must be transported promptly and maintained in a manner that allows survival of fastidious organisms and prevents overgrowth by more hardy organisms.
-
Specimens that are collected in syringes are best maintained by dead-capping the syringe, expelling excess air, and transporting to the laboratory in the syringe.
-
A fluid or tissue specimen is generally a more desirable specimen than a swab. Each tube or container with obtained specimen must be provided with a labelling tape- with written name of the patient, date of taking the specimen and exact description of the source of the specimen. Other details to be noted are: provisional diagnosis, date (hour) of taking it and sending to the lab, requested examination etc.
Clinical Specimens
Following are the clinical specimens that can be collected for diagnosis of microbial diseases:
-
Blood
-
Urine
-
Sputum
-
Stool CSF
-
Conjunctival swab
-
Ear discharge
-
Skin
-
Throat swab
-
Pharyngeal swab Vaginal swab
-
Urethral discharge
-
Biopsy specimens
-
Pus
-
Aspirated materials
Collection of Individual Specimen
-
Collection of Blood: Blood for analysis may be obtained from veins, arteries or capillaries. Venous blood is usually the specimen of choice. The vein from which the blood is to be taken should be clearly seen and the skin overlying the vein is vigorously wiped with 70% alcohol. Blood is collected by strict aseptic technique and care should be taken to avoid introducing organisms into the blood stream as well as prevent contamination of the specimen.
-
Collection of Urine: The type of urine specimen to be collected depends upon the tests to be performed. Random urine specimens are suitable for only a few tests. The peri-urethral area is cleaned twice with soap and water. The urethra is flushed by voiding some urine which is discarded. The subsequent mid stream urine is collected directly in a sterile container and is used for culture and colony counting.
-
Collection of Sputum: It is collected in a clean, dry, wide necked, leak proof container. The subject is asked to cough deeply to produce a sputum specimen. During its collection, adequate safety precautions must be taken to prevent the spread of infectious organisms and to avoid contaminating the outside of the container.
-
Collection of Stool: stool is passed directly into a sterile, wide-mouth, leak-proof container with a tight fitting lid. Stool for examination of ova and parasites should be placed in preservative immediately after the collection.
-
Collection of CSF: CSF must be collected aseptically to prevent the entry of organisms into the central nervous system. The fluid is usually collected from arachnoid space. A sterile wide bore needle is inserted between the fourth and fifth lumbar vertebra and the CSF is allowed to drip into a dry sterile container. The samples are immediately delivered with a request form to the laboratory.
-
Specimen collection with Conjunctival swab: Any visible purulent conjunctival discharge is collected on a swab and inoculated at once for culture.
-
Specimen collection with Ear swab: Ear swab can be used to collect material from the external ear. The swab on the wire is inserted into the external auditory canal with a twisting motion to collect a secretion from it.
-
Specimen Collection from Skin: The area of the skin from which specimen is collected is first cleaned using soap and water. Swabs are firmly rubbed over the affected part of the skin and sent at once to the laboratory for processing.
-
Specimen collection with Throat swab: Depress the tongue with a tongue depressor. Introduce the swab between the tonsillar pillar and behind the uvula without touching the lateral walls of the buccal cavity. Any exudates or membrane should be taken for specimen.
Transportation of Specimen
Specimen should be well packed and labelled. The specimen must be delivered to the laboratory as soon as possible. In case of any delay, transport media, refrigeration, freezing may be used.
Normal Flora
The microbes that live inside and on top of human bodies are referred to as normal microbial flora. These live on healthy, normal people's skin and mucous membranes. In a healthy human under normal circumstances, these flora are safe and might even be helpful.
Role of Normal Flora
Beneficial role:
-
Possible role in human nutrition and metabolism:
-
Synthesis of vitamin K- by Escherichia coli in intestine
-
Synthesis of vitamin B- by Pseudomonas in intestine
-
Prevent the entry of pathogens in the body.
-
Helps in stimulation of immune system
Disease production:
-
Normal flora may act as opportunistic pathogen when resistance of the host is lowered.
-
They act as pathogens outside their normal habitat. eg. E. coli in urinary tract cause infection.
| Location | Name of Normal Flora |
|---|---|
| Skin | Staphylococcus epidermidis, Diphtheroids |
| Conjunctival sac | Corynebacterium xerosis, Staphylococcus epidermidis |
| External Auditory meatus | Staphylococcus epidermidis, Diphtheroids |
| Oral cavity |
Peptostreptococcus, Anaerobic Streptococcus, |
| Upper respiratory tract | Diphtheroids, Staphyllococci, Corynebacterium |
| Gasto-intestinal tract | Lactobacilli, Escherichia coli, Klebsiella |
| Vagina | Lactobacillus, Enterococcus E. coli, |
Concept of opportunistic and pathogenic organisms
Both of these organisms cause disease but under different conditions of the host.
Opportunistic Organisms
These creatures are typically found in humans or environments where they coexist peacefully with their hosts. These organisms multiply and have the potential to spread disease when the human (host) immune system is compromised in any way. Pathogens (bacteria, viruses, fungi, and protozoa) that take advantage of an organism's compromised immune system or altered anatomical location produce opportunistic infection. For instance, AIDS patients are more prone to pneumonia and TB. E. coli lives in the large intestine without harm, but it causes urinary tract infections in the urinary system.
Some opportunistic organisms include:
-
Aspergillus sp.
-
Candida albicans.
-
Cryptococcus neoformans.
-
Cryptosporidium.
-
Cytomegalovirus.
Pathogenic organisms
These microorganisms have the ability to sicken their host. A human pathogen is one that can make people sick. Pathogenic organisms are any organisms, such as viruses, bacteria, fungus, or parasites, that harm their host (people, animals, or plants). (Unit 1, under the heading "classification of microbial diseases," lists pathogenic organisms and the diseases they cause.) Specific strains of bacteria like Salmonella, Listeria, and Escherichia coli, as well as viruses like Cryptosporidium, are frequent examples of harmful organisms.
Drug Resistance
It is the decline in a drug's ability to treat illness or control symptoms. The ability of pathogens (such as viruses, bacteria, parasites, etc.) to proliferate despite the presence of medications that would typically cause the organisms to die or restrict their growth is known as drug resistance. A significant issue in antimicrobial therapy is the rise in drug-resistant microorganisms. Drug resistance is more or less common depending on the organism and antibiotic used.
Drug resistance is of two types:
-
Primary resistance: Some bacteria possess an innate property of resistance to certain drug. eg. Resistance of E. coli to penicillin.
-
Acquired resistance: It results either from mutation or gene transfer. Pseudomonas aeruginosa are resistant to Tetracycline.
Mechanism of Drug Resistance
Drug resistance may be due to following factors:
-
Permeability of cell wall: Microorganisms change the chemical nature and thus permeability of cell wall to the drug and become drug resistant. eg. Pseudomonas aeruginosa are resistant to Tetracycline.
-
Production of Enzymes: Some bacteria such as Staphyllococci produce the enzyme beta-lactamase which destroy the drug. This is the reason penicillin resistant. that Staphyllococci are
-
Altered metabolic pathway: By changing the metabolic pathway, some bacteria bypass the reactions inhibited by the drug. eg. Some bacteria are resistant to drug Sulphonamide because they utilize preformed folic acid and do not need the synthesis of folic acid from PABA (para- aminobenzoic acid).
ANTIBIOTIC SENSITIVITY TESTS (AST)
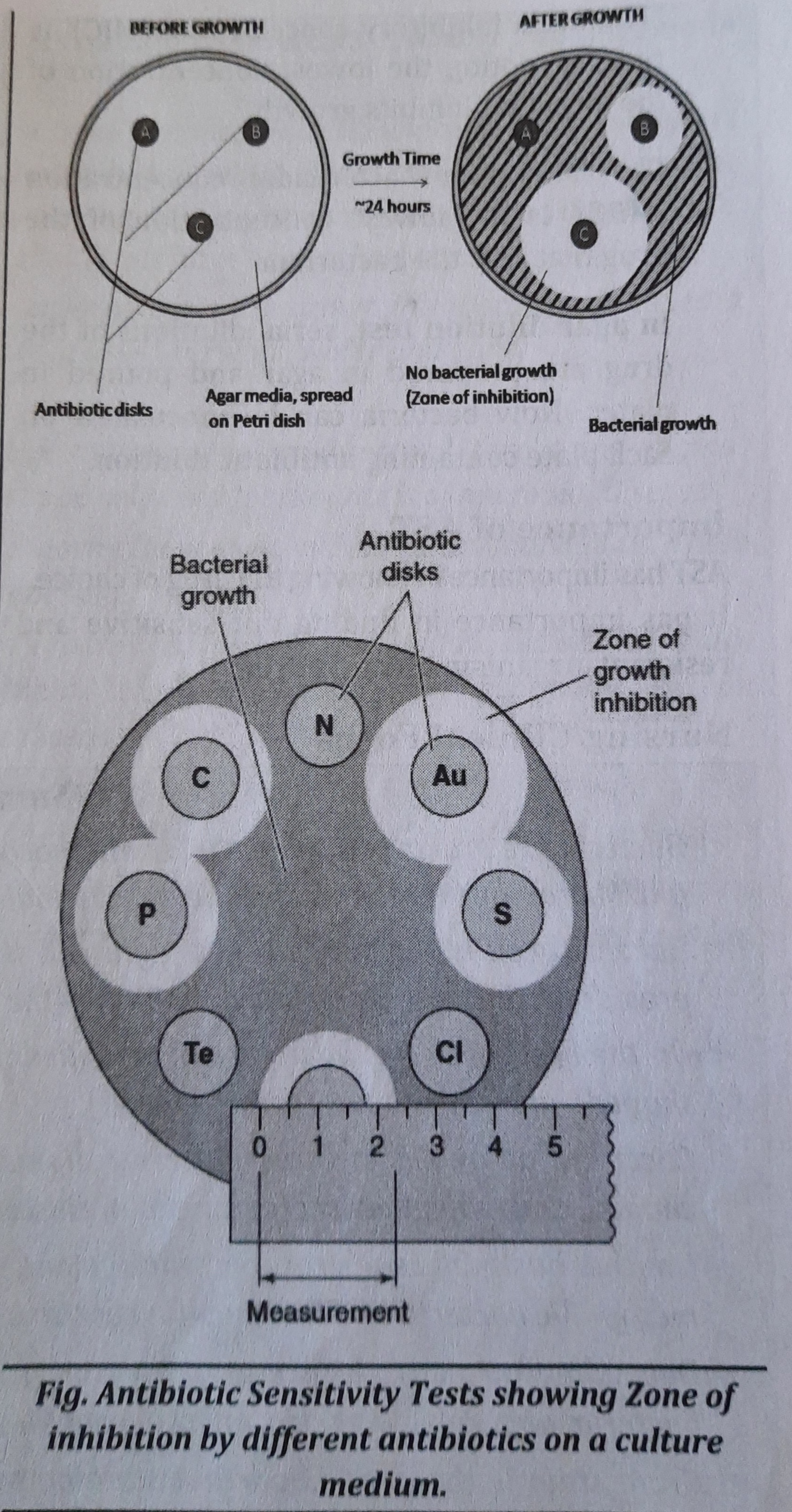
Pathogenic bacteria show great variations in susceptibility to antibiotics. Therefore, it is essential to determine the susceptibility of pathogenic bacteria to antibiotics. This is called Antibiotic sensitivity test.
It is classified into two types:
-
Diffusion test
-
Dilution test Diffusion test (disc diffusion test or
Kirby-Bauer disc diffusion test
In this method, the drug is allowed to diffuse through a solid medium. The concentration of drug is the highest near the site of application of the drug and decreases with distance. The test bacterium is inoculated on the medium and its sensitivity to drug is determined from the inhibition of its growth. This test is usually performed by disc diffusion method which involves the use of filter paper disc impregnated with antibiotics.
Procedure for disc diffusion method:
-
A suitable dilution of bacterial culture in broth is flooded on the surface of solid culture medium or inoculated on the surface of solid culture medium by spreading with swabs. The solid culture medium used more frequently is Mueller Hinton agar or Nutrient agar.
-
The culture plates are dried at 37°C for 30 minutes.
-
The antibiotic discs are applied in a number of four to five in a 10 cm culture plate
-
The plates are incubated at 37°C for whole night and observed for Zone of inhibition of growth around the disc.
-
The diameter of zone of inhibition is measured.
-
Growth will be inhibited around the disc antibiotics to which the containing antibiotics bacterium is susceptible, but not around those to which it is resistant.
-
The results are reported as 'sensitive', 'moderately sensitive' or 'resistant to the different drugs.
Dilution test
In this method, the serial dilutions of the drug are prepared and inoculated with test bacterium. Dilution test is performed by two methods: tube dilution test or agar dilution test. In tube dilution method, serial dilution of the drug in broth are taken in tubes and a standardized suspension of test bacterium is inoculated. After overnight incubation, the "Minimum inhibitory concentration(MIC)' is read by noting the lowest concentration of the drug that inhibits growth. The 'Minimum bactericidal concentration (MBC)' is the lowest concentration of the drug that kills the bacterium. In agar dilution test, serial dilutions of the drug are prepared in agar and poured in plates. Now bacteria can be inoculated on each plate containing antibiotic dilution.
Importance of AST
AST has importance in knowing the drug of choice. It has importance in finding out sensitive and resistant organism towards drug.Nursing/ Clinical Focus
Note:
-
MIC (Minimum Inhibitory concentration)
MIC is defined as the lowest concentration of drug that inhibits the growth of the organism. It provides knowledge to the physician with exact concentration of drug to guide the choice of both the drug and the dose. -
MBC (Minimal bactericidal concentration):
It is important to know the minimum concentration of drug that actually kills the organism. This concentration is called MBC.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google