Pyloric Stenosis
Subject: Child Health Nursing

Overview
Pyloric stenosis is a disorder in which the stomach narrows into the small intestine (pyloric), resulting in projectile vomiting. The circular muscle of the pylorus has hypertrophy, creating gastric outlet obstruction. It is unclear if this is a true congenital constriction or a functional hypertrophy of the muscles that occurs in the first few weeks of life. In the first few weeks following birth, the newborn is asymptomatic. Symptoms commonly appear in the second week of life. Vomiting: curdy type vomiting occurs after nursing and eventually rises in frequency and becomes projectile (1-2weeks). After vomiting, the newborn appears to be in good health and eager to breastfeed again. The exact origin is unknown; however, the underlying cause may be inherited- several members of a family may have had this problem when they were young. Surgery is the preferred treatment for pyloric stenosis. Pyloromyotomy is conducted by an incision in the right upper quadrant. A longitudinal incision is made into the pylorus circular muscle but not into the submucosa.
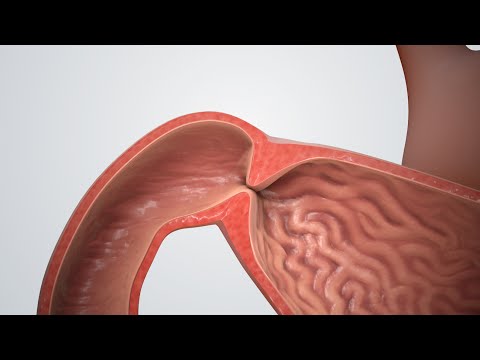
Pyloric stenosis is a disorder in which the stomach narrows into the small intestine (pyloric), resulting in projectile vomiting. The circular muscle of the pylorus has hypertrophy, creating gastric outlet obstruction. It is unclear if this is a true congenital constriction or a functional hypertrophy of the muscles that occurs in the first few weeks of life.
Causes
- Unknown
- Inherited- several members of a family may have had this problem in infancy
- Monozygotic twins
- Congenital (unclear)
- Acquired: maternal stress in the last trimester of pregnancy elevated prostaglandin level, deficiency of nitric acid and an immature pyloric ganglionic cell may facilitate stenosis.
Pathophysiology
Abnormal muscular layer development causes hypertrophy and hyperplasia of the pyloric muscle, resulting in thickness and narrowing of the pyloric canal and eventually preventing food from flowing from the stomach to the intestine. As a result of the accumulation of food material within the stomach, the youngster will have a dilated stomach.
Clinical Manifestation
- The newborn is asymptomatic in the first weeks after birth. Symptoms develop usually 2nd week of life. Common symptoms are:
- Vomiting: curdy type vomiting occurs after breastfeeding gradually increases frequently and becomes projectile (1-2weeks). Newborn looks well after vomiting and eager to breastfeed again.
- The presence of upper abdominal distension.
- Palpable olive-shaped mass is found in epigastrium jut to the right of the umbilicus.
- Gastric peristaltic wave is visible moving from left to right across the epigastrium.
- Decreased frequency and volume of stool.
- Sign of dehydration and electrolyte imbalance.
- The newborn has a weight loss, failure to thrive.
Diagnosis
- Complete history and physical examination to find out presentation of an infant.
- Ultrasonography of upper GI tract.
- Serum electrolyte (sodium, potassium) level, hemoglobin level.
Therapeutic Management
An surgery is used to treat pyloric stenosis. However, before undergoing surgery, the baby's general problems, such as dehydration and electrolyte imbalances, must be addressed.
- Obtain IV access and administer a 20ml/kg normal saline IV bolus. Then, at 150% maintenance volume, give 5% dextrose with 1/2 normal saline. Over the course of 24 to 48 hours, correct fluid and electrolyte imbalances. Establish a good urine production (> 1 ml/kg/hour) before adding potassium and chloride to the intravenous fluids as directed.
- Pyloromyotomy surgery is performed under anesthesia at the age of 4-5 weeks. Tight pyloric muscle is repaired in this surgical procedure by dividing the pylorus muscle to open the gastric outlet.
- Isotonic saline gastric lavage
- Begin feeding with clear liquids for the first 24 hours after surgery, then advance to modest amounts of glucose water or electrolytes solutions on a regular basis. Most babies will be eating normally by the time they go home, which is two to three days following the surgery.
- Antibiotic treatment
Nursing Management
Preoperative care
Preoperative emphasis should be for restoring of fluid and electrolyte balance.
- Monitor feeding pattern and the association between feeding and vomiting.
- Assess the amount o, character, and frequency of vomiting.
- Monitor vital signs, intake output, general condition
- Keep infant NPO, nasogastric tube drainage
- Promote adequate hydration and nutrition by administering parental fluids and electrolyte as prescribed.
- To prevent aspiration
- Feed the infant slowly
- Perform burping after feeding
- Position the infant in the high fowler position on the right side after feeding.
- Prepare for the surgical procedure.
Post – operative care
- Assess wound site, vital signs and other general condition after surgery.
- Promote comfort with analgesic, cuddling, holding by parents.
- Care of operation site consists of observation of incision site for bleeding, drainage, inflammation and care of the incision site.
- Start feeding 4-6 hours after surgery with clear fluid. If tolerated, advance to breast milk usually after 24hours.
- Encourage the parents to remain with their child, involve in their child care.
- Support and reassurance of the parents.
- Discharge after 48hours after achievement of feeding regimen.
- Provide instruction about home care like frequent feeding, positioning, burping after feeding, wound care follow-up care as well as other well baby care.
Things to remember
- Pyloric stenosis is a disorder in which the stomach narrows into the small intestine (pyloric), resulting in projectile vomiting.
- The circular muscle of the pylorus has hypertrophy, creating gastric outlet obstruction.
- It is unclear if this is a true congenital constriction or a functional hypertrophy of the muscles that occurs in the first few weeks of life.
- Inherited- many family members may have had this condition as children.
- Surgery is the preferred treatment for pyloric stenosis. Pyloromyotomy is conducted by an incision in the right upper quadrant. A longitudinal incision is made into the pylorus circular muscle but not into the submucosa.
Questions and Answers
What are the treatment and nursing management of pyloric stenosis?
Therapeutic Management
General management of newborn includes:
- Utilizing IV fluids to control hydration and nutrient levels.
- Controlling aspiration.
- The preferred course of treatment for pyloric stenosis is surgery. Through the incision in the right upper quadrant, a pyloromyotomy is carried out. The pylorus's circular muscle is cut longitudinally, but not all the way through to the submucosa.
- Infants with IHPS have laparoscopic surgery, which results in a brief hospital stay and a speedy recovery.
Nursing management
Preoperative care:
The restoration of fluid and electrolyte balance should get priority during preoperative care.
- Keep an eye on your eating habits and any correlation between eating and vomiting.
- Analyze the volume, kind, and frequency of vomiting.
- Watch your vital signs, your intake, and your general health.
- Maintain the infant's NPO and nasogastric tube drainage.
- Promote proper nutrition and hydration by giving parents the recommended amounts of water and electrolytes.
- Avoiding aspiration.
- Feed the baby gradually.
- After eating, perform burping.
- After feeding, place the baby on his or her right side in the high fowler position.
- Make sure you're ready for the surgery.
Post – operative care:
- After surgery, evaluate the wound site, vital signs, and other aspects of general health.
- Encourage comfort with analgesics, snuggling, and parental holding.
- Observing the incision site for bleeding, drainage, inflammation, and wound care comprise the care of the operation site.
- Start feeding with clear fluid four to six hours following surgery. Advance to breast milk usually after 24 hours, if tolerated.
- Encourage the parents to take an active role in their child's care and stay with them.
- Parents' support and reassurance
- 48 hours after achieving the feeding schedule, discharge.
- Give instructions on how to care for a baby at home, including frequent feeding, positioning, burping after feeding, wound care, and other well-baby care.
List the causes of pyloric stenosis.
- Unknown
- Several family members may have experienced this issue in infancy due to inheritance.
- Monozygotic twins
- Congenital (unclear)
- Acquired factors that may contribute to stenosis include maternal stress during the final trimester of pregnancy, an increase in prostaglandin levels, a lack of nitric acid, and an immature polyric ganglionic cell.
Define pyloric stenosis.
Projectile vomiting is a symptom of the illness known as pyloric stenosis, which is a constriction of the stomach into the small intestine. The pylorus's circular muscle has grown larger than normal, obstructing the stomach's outflow. The difference between a functional muscle hypertrophy that appears in the first few weeks of life and a true congenital constriction is unclear.
What are the sign and symptoms of pyloric stenosis?
- In the initial weeks following delivery, the newborn exhibits no symptoms. In the second week of life, symptoms typically appear. Common signs include:
- Vomiting: Following breastfeeding, curd-type vomiting increasingly becomes more frequent and projectile in nature (1-2weeks). After throwing up, the newborn appears healthy and is anxious to nurse once more.
- Upper abdominal distension is present.
- Just to the right of the umbilicus, in the epigastrium, is a palpable mass that resembles an olive.
- Moving over the epigastrium from left to right is a gastric peristaltic wave.
- Decreased stool frequency and volume.
- Indication of electrolyte imbalance and dehydration.
- The newborn is underweight and struggling to grow.
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google